When and how should a child’s temperature be taken?
This is possibly one of the most unclear topics in the field of pediatrics. There are quite a few techniques and devices, and each have their own advantages and disadvantages.
Let me start by saying that the most reliable temperature readings in children are the ones taken rectally, using a mercury thermometer.
However, taking a rectal temperature may be unpleasant, and completely irrelevant when it comes to older children. Additionally, mercury thermometers are no longer used in most countries due to the concern of mercury poisoning.
So, should a rectal reading be taken regardless? Or there is a better technique? Should a digital thermometer be used? Should it be placed under the armpits or under the tongue?
Furthermore, is it important to determine the exact temperature of the child? And what about other devices – ear thermometers and that sort of stuff? Or maybe an experienced mother’s hand is better than all these devices put together?
To find out the answer to all these questions and more, continue reading below.
Should a child’s temperature be taken?
If you are concerned that your child might have fever, the right thing to do is to take their temperature in order to get a reliable answer and find out whether or not they have fever.
Often, a child may feel warm to touch but the thermometer reveals that they do not have fever. The opposite could happen as well, where a child feels slightly warm but the thermometer reveals a very high temperature.
However, is it important to determine the exact temperature or is it enough to just check how the child feels to touch?
The answer to this, as I suggested earlier, is to take the child’s temperature at least once during an illness in order to get a reliable answer to whether or not they have fever.
When should a child’s temperature be taken?
Or in other words, is it important to run after your baby, who has been ill for 3 days, with a thermometer and take their temperature every two hours?
I really don’t think so.
If the parents have taken the baby’s temperature and have found out that he has a high fever, then in my opinion it is unnecessary to take the temperature every 4 hours and it is okay to give the child anti-pyretic based on the time intervals or how warm he feels to touch.
When talking to experienced mothers in my clinic, I usually ask them to categorize the child’s temperature by telling me whether he has ‘no fever’, a ‘slight fever’ or ‘boiling’ to touch.
And what about the exact number? Again, the exact number is not useful in guiding me towards the diagnosis.
Okay, so how should a child’s temperature be taken?
Touching the forehead
Touching a child’s forehead using the back of the palm can provide experienced parents with general information as to whether or not a child has fever and whether the fever is high.
I must say, as I mentioned earlier, that as a pediatrician who has assessed lots of children with fever, in most cases it is important for me to know whether or not the child had fever and whether it was very high. The precise number is not so important. That is why I do not think that determining whether a child, who has been ill for a few days, has fever by touching their forehead, is wrong. I do suggest getting a reliable reading using a thermometer at least once during the beginning of the illness.
Mercury thermometers
In most countries, medical devices containing mercury are prohibited. Despite mercury thermometers being the most accurate technique, it is irrelevant nowadays.
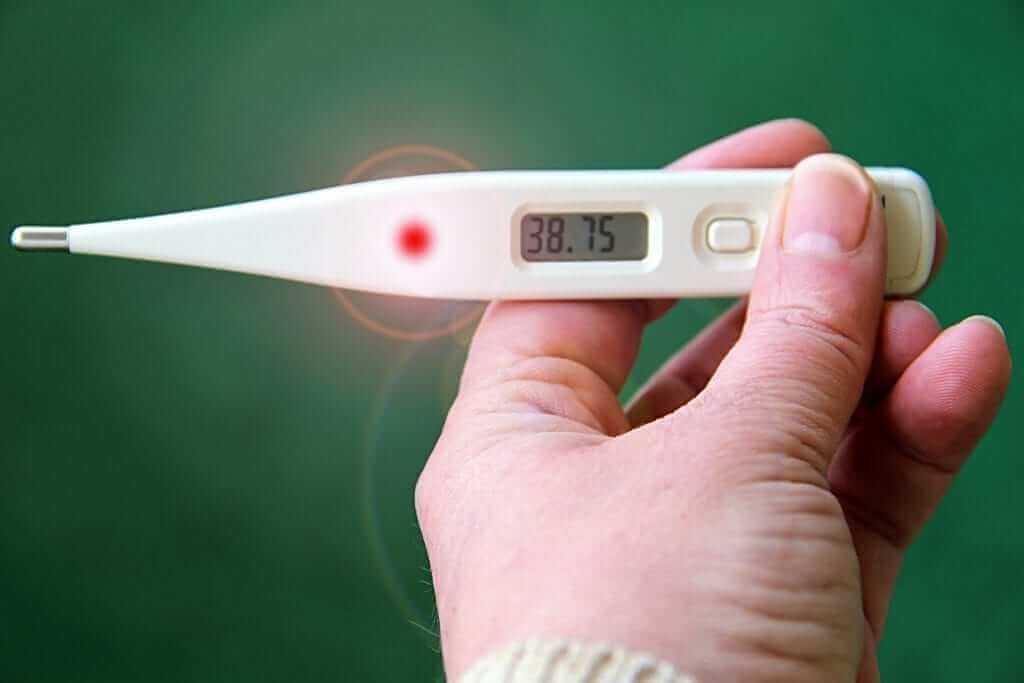
Digital thermometers
These devices are the current alternative to the old mercury thermometers and are the most recommended nowadays. Among their advantages are how quickly a reading is provided and the reliability of this reading (depending on the temperature being taken, as I will explain later).
Pacifier thermometers
Not accurate at all. These are not recommended.
Forehead sticker thermometers
Not accurate at all. These are not recommended
Infra-red forehead thermometers
Their advantage is obviously how fast a reading is provided but the disadvantage is the price and the reliability of the reading.
In practice, these can be used as an alternative to the digital thermometers despite the fact that the reliability depends on the correct placement of the thermometer by the parents.
Where should a temperature be taken in children?
It is well-known and obvious to everyone that there are differences in the temperatures taken at different sites in the body.
The most reliable readings are those taken rectally (through the anus) but lots of parents take temperature in the mouth, armpits and ears.
Rectal temperature readings
Rectal readings are considered the most reliable but it is a good method mainly for babies and young children.
Following disinfection of the thermometers (it is recommended to disinfect before and after every use), using alcohol (you can use the 70% alcohol used for disinfecting the umbilicus), the tip of the thermometer should be pulled using a lubricant (any diaper ointment can be used).
The thermometer should be gently pushed into the anus up until the depth required, as indicated by the line on the thermometer.
For small babies this can be done when they are in the position placed when their diaper is being changed. Bigger babies can be placed on their abdomen with their knees folded towards their bodies or can be laid on their side.
The duration of the reading varies depending on the device. Digital devices will beep when the reading appears.
Make sure to label your thermometers so that you don’t use the same thermometer for rectal measurements and other sites in the body…
What is the age cut-off for rectal readings?
There is not specific cut-off. It is obvious that in younger babies this is the most reliable and easiest method, but I do not think there is a specific age when you should stop using this method. It is believed that rectal readings are preferred up until the age of 3 years but I don’t think I prefer rectal readings even in children younger than that age. Of course, rectal readings should definitely not be taken for children that are older than 3 years.
Oral temperature readings
Readings taken in the mouth are less reliable than rectal readings and usually the temperature taken in the mouth is about half a degree less than that taken rectally. Oral readings require a certain level of cooperation of the child as the mouth needs to be closed with the thermometer underneath the tongue while the temperature is being taken. It is difficult to get that level of cooperation in a child younger than 5 years and therefore this method is not recommended in young children. Additionally, it is important to wait for about 10 minutes after drinking/eating and before taking oral temperatures.
Make sure to label your thermometers so as not to use the same thermometer you used to take an oral reading to take a reading elsewhere in the body.
Armpit temperature readings
Similarly, to oral temperature readings, this reading is less reliable than the one taken rectally and usually the temperature in the armpit is about half a degree lower than the one taken rectally. Nonetheless, in neonates, armpit readings are considered reliable, possibly equally reliable to rectal readings. Make sure to press the child’s arm to their body so that the thermometer touches the skin of the child for the duration of time required for the reading.
Temperature readings in children in the ear or forehead using digital devices
This is the easiest and simplest method to take temperature readings but also the most expensive, and is not really accurate.
Not once have I encountered parents who claim that the digital thermometer showed a reading in one ear that was substantially different than the reading in the other ear. It seems like the forehead thermometers are more reliable than devices used in the ear (whose reliability depends on the proper placement of the device exactly opposite to the ear drum).
I think these devices are good especially for parents who:
– Deep down in their hearts know that their child does not have fever and just want to make sure of it (despite these devices being inaccurate they don’t usually indicate fever when the child’s temperature is normal).
– Know that their child has fever, and the use of the device is just an alternative to making an assessment based on touch, when the exact temperature is not so important. Again, it is usually just important to determine whether or not there is a fever, and if so, whether or not it is high.
To summarize, each person can find the method or technique that best suits their baby/child, having understood the advantages and disadvantages of all the different methods out there.
For comments and questions, please register
