
Bacterial skin infections
A very important chapter in pediatrics, about different skin infection caused by many bacteria. Although my focal point of view is on children, there are a lot of adults with these types of infections, so it is important for them to read and understand this post as well.
What is important to understand before beginning reading?
– This post is about acute infections, and not chronic ones. This means someone who was healthy yesterday and today had a skin infection, and not for those with long, ongoing skin conditions.
– There are many types of infections, and we all have a lot of skin. There for – there are many types of skin infections. Some are very common, some are rare. This post will focus on the more common infections.
– Not only common bacteria cause skin infections but also viruses, fungi or other rare bacteria. This post is about common bacterial pathogens.
What are the most common pathogens causing skin infections in children and adults, and how does it affect the treatment?
We should all know two bacteria which we all carry on our skin, and they are accountable for most of skin infections in all ages:
Staphylococcus aureus: the most common bacteria to cause skin infections, which we all carry on our skin from birth till’ 120 years. Sometimes, the balance in which we live in with Staph aureus is interfered, and this imbalance may cause skin infections. This bacterium is resistant to simple penicillin, and must be treated with broader spectrum antibiotics. In the case of ‘simple’ methicillin-susceptible Staphylococcus aureus (called also MSSA), a group of antibiotics called Cephalosporin, mainly its first generation (which is basically upgraded penicillin), are great for this bacteria. This antibiotic is called Cephalexin, and it is the “go to” drug when it comes to skin infections. However, there are some strains of Staph aureus that developed resistance to this antibiotic (methicillin-resistant Staphylococcus aureus or MRSA), and in those cases, the use of a different antibiotic is warranted. Your pediatrician should know the epidemiology of the local bacteria and would decide which antibiotic to prescribe, of needed (see more in the treatment section below).
Group A streptococcus: the same Strep that causes acute pharyngitis. Group A strep is sensitive to many different antibiotics, including simple penicillin. If it is susceptible to penicillin it is most likely susceptible to first generation cephalosporin.
There for – first generation cephalosporin (mainly Cephalexin), is the go to drug for skin infections in many parts of the world. Those of you given different drugs like Amoxicillin and Clavulanate, second generation Cephalosporin or other choice, can ask your physician why, since there should be a good reason for that choice. Just remember that Cephalosporin cannot be prescribed to those with severe allergy to penicillin.
What are the different layers in the skin, and what are the possible infections?
Imagine an intricate layer cake. This is the way our skin is formed.
The upper and visible part is called Epidermis. A simple and shallow infection in this layer would be called Impetigo.
The next layer is the Dermis. This layer also inhibits the hair follicles. An infection involving the upper part of the dermis (and off course the epidermis above it), would be called erysipelas. An infection of the deeper layer of the dermis and the fat layer beneath it is called cellulitis. A localized infection around and in the hair follicle would be called folliculitis.
The next layer is the fascia and the muscles beneath her – infection in these deep layers would be called fasciitis or myositis. These are severe infections which are less common, and would not be discussed in this post.

What is Impetigo:
The most common skin infection in children (involving only the epidermis). It is so common that there is another post dedicated especially for it (read about it here).
What is Erysipelas:
An infection involving the dermis and epidermis, which is not that common in children. The area of infection is warm, sensitive to touch and there is redness with marked and elevated borders. Systemic signs of infection (including fever) are common.
This infection is more common in adults because of chronic skin conditions, venous insufficiency and obesity. In children we can see this infection now and then, mostly in adolescence with poor podiatric hygiene. The bacterium (Group A strep) enters through the lesioned skin and cause infection. It is most often seen in the front of the shin.
Oral antibiotic therapy is needed, sometimes even intra venous (IV) therapy with close monitoring. Elevating the feet and warm compresses could help.
Those who suffered from erysipelas once are prone for recurrent events, and therefore, in cases like this (which are rare in children) there is room for consultation with a specialist in this area, for preventing recurrences.
What is Folliculitis:
An infection around the hair follicle, mostly caused by Staph aureus. The lesions are small, separated from one another with a red based and an elevated center (see the picture). Common in the buttocks area, with poor hygiene and shaving as the main risk factors.
What is Cellulitis:
An infection of the deep layers of the skin, involving mainly the dermis, and less of the epidermis. Very common in children. Similar in the clinical presentation to erysipelas – warm to touch, sensitive and with redness in the area (but with less marked borders). Fever is sometimes present.
Cellulitis is common in children, with many different causes which are mainly impairment of the skin’s integrity. Sometimes there is a clear story (a cut or insect bite who got infected), and sometimes there is micro lacerations that were unnoticed. Every area in the body could be involved, in children the limps are more common.
The most common bacteria responsible is again, Staph aureus.
Depending on the extant of the finding and whether there are systemic symptoms, a decision on antibiotic treatment would be made. Elevating the leg and using warm compresses could help. With the right treatment there will be no scars or long term problems.
Notice the center of the area – cellulitis could be a reaction to a focal infection (like a furuncle or abscess). In these cases, drainage of the lesion should be considered.
What are Abscesses, Furuncles and Carbuncles:
When bacteria, mostly Staph aureus, is going deeper inside the skin layers it can cause an abscess (a collection of pus with an inflammatory reaction around it, sometimes cellulitis), a furuncle (an infection surrounding the infected hair follicle), or carbuncle (a cluster of furuncles).
The beginning of the process can be a simple infection gotten worse, or deeper infections. It can start spontaneously without an apparent cause like a bruise, abrasion or insect bite.
The clinical signs are redness and extreme tenderness (sometimes suggesting that secondary cellulitis may be present). Usually there is a center with a collection of pus. Note that although locally there is a severe infection most often there will be no systemic fever.
In cases of skin infections like these, treatment should be given fast, to prevent exacerbation of the infection. There is room for using anti-septal scrub (like chlorhexidine), draining the abscess and considering systemic antibiotic treatment.
The healing process may leave a scar, so it’s important not to fiddle with the wound too much.
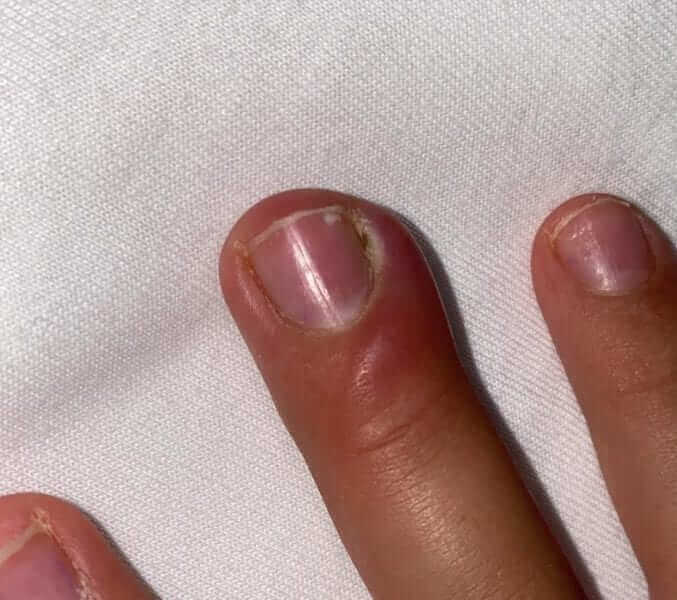
What is Paronychia:
A very common infection in children, there for it deserve a special attention in this post. The location of the infection is at the joint of the nail to the skin. It sometimes occurs after local trauma or peeling of the skin in this area.
The area is swollen, red and tender, a bit warm to touch (see the picture below). It is common to see pus accumulating. In most cases local treatment does the trick – using warm compresses to soften the skin and applying local antibiotic ointment. Sometimes there is need for opening and draining the area. I suggest not to do this alone at home, since there is a specific technique in doing so.
Oral antibiotic treatment is usually not necessary, except for severe cases in which the infection was not given the appropriate treatment early enough.

What are the treatment principles in skin infection in children?
It is hard to make an overall statement for all skin infections. That is because every case is a bit different. Treatment decisions are based on the state of the child, systemic and local symptoms, as well as factors relating to his previous medical history. For example, in a case of folliculitis I would recommend a local antibiotic cream, while for cellulitis with 39.0 fever, I will choose a systemic antibiotic.
There is an importance in knowing the options of treatment:
Compresses: a warm compress is always good to do on an infected area. It can soften an area with puss and bring to a better drainage. Another treatment which is better than compresses is to soak the inflamed area with water and anti-septic soap.
Drainage: with a simple technique (squeezing the area), half-surgical (using a needle) or surgical (a scalpel). This is a number one rule in medicine – abscesses needs to be drained to show improvement. This means, that if there is pus inside an abscess which has not been drained, applying local antibiotics or taking oral antibiotic treatment would not help. Is can calm the inflammation but will not solve it. I do not suggest parents to walk around with needles in their houses, draining wounds. But after a warm bath and tendering of the skin, you can squeeze the area gently to see if the pus comes out, which can help the healing processes. Drainage by needle or scalpel must be done by a physician.
Local antibiotics: with or without bandages, it is very helpful for focal, shallow infections. It is not as helpful with deep tissue infections (such as cellulitis, erysipelas, act), but can assist as adjuvant therapy. When there is worry that the child would get the antibiotic cream on his cloths or bed sheets, the area must by covered in bandages at least 3 times a day, to give it a chance to work.
Systemic antibiotics: in some cases there is no need for systemic antibiotics, for example – paronychia. In other we will defiantly use antibiotics, for example cellulitis. In either case of severe skin infection (or even more, if the child has a fever), go see your physician to decide on systemic antibiotics. Remember that the first line antibiotic is places when MRSA is rare is first generation Cephalosporin. If the physician prescribes something else – ask why. Remember that in severe cases the doctor can recommend hospitalization and IV antibiotics. The length of treatment varies from case to case and is about 5-14 days.
What to do with recurrent skin infections?
Besides impetigo, which has a tendency to recur, most skin infection will be a onetime thing. Having said that, if it does recur, your physician will probably think about several things.
So, please read carefully the dedicated chapter for recurrent skin infection in children.
In summary:
Alhough this post has a lot of information, it fails to describe all of the skin infections pediatricians meet every day. What about perianal strep infection? And periorbital cellulitis? What about recurrent abscesses in the groin area (Hidradenitis Suppurativa)? And many more.
So in these specific conditions, a more specific specialist should be consulted.
So this is it for now. I wish you a good day and a whole, non-injured skin.
For comments and questions, please register
