
The vaccine for Human Papillomavirus (HPV) – Gardasil 9
Most vaccine schedules for children and adolescents around the world include the vaccine against Human Papillomavirus, named Gardasil 9.
Even though it’s been a few years now since the introduction of this vaccine, the vaccine itself still raises concern and its efficacy is largely questioned among the general public – why vaccinate? Is it only for girls? Why should boys be vaccinated? Why specifically administer is at such a young age? These concerns lead to low compliance in some countries in the school-age group (as low as 50%).
Therefore, the aim of this chapter is to answer all those questions that’s I’ve been tackled with by you, regarding this vaccine.
What is the Human Papillomavirus? And how does it affect humans?
The Human Papillomavirus is a common virus that is transmitted mainly through sexual contact. In fact, it is the most common sexually transmitted infection in the world.
Approximately 80% of sexually active men and women will eventually get infected with one of the strains of the virus throughout their lifetime.
Usually, the transmission is asymptomatic and therefore an individual who is infected is usually unaware of this and does not realize that he/she could potentially infect others. When it comes to clinical manifestations, the virus can cause warts in the genitals, precancerous lesions (in the vulva, vagina and cervix), and cancerous lesions (in the vulva, vagina, cervix, anus, mouth and throat), in women.
In men, it can lead to development of warts in the genitals, precancerous lesions (in the anus) and cancerous lesions (penis, anus, mouth and throat).
How is this virus related to cancer and how can a virus cause cancer?
After transmission, the papilloma virus is able to enter the cells in the body (such as cells in the cervix), and cause them to replicate excessively. It can lead to uncontrolled division of cells and their conversion to cancerous cells.
How is the virus transmitted from one person to another?
The transmission occurs through direct contact, mainly during vaginal sexual intercourse, anal sex and oral sex. The use of condoms greatly reduces the risk of transmission but does not completely prevent it.
What’s the deal with the different types of HPV?
The papilloma virus is actually a general name given to a family that includes about 200 different strains. The majority of strains do not cause disease. Some of the strains can cause development of warts in the genitals in both men and women. These are designated “low risk” strains. Of these, two, namely HPV type 6 and 11, cause 90% of the genital warts found in men and women.
Other strains, however, can cause different types of cancers and are therefore referred to as “high risk” strains. For example, HPV type 16 and 18 are responsible for about 70% of cervical cancer cases and 85% of anal cancer found in men and women.
How prevalent is HPV around the world?
As estimated by the WHO, the worldwide prevalence of HPV among women is 11.7%. Among men, the estimated prevalence is higher, about 21%.
The HPV virus is responsible for 99% of cancers in the cervix and uterus. Approximately 530,0000 new cases of cervical cancer develop every year, leading to about 266,000 deaths.
What type of vaccine is the HPV vaccine?
The only vaccine available today, Gardasil 9, is made up of particles that resemble the virus and its surface protein. It does not contain the virus’ genetic material and therefore cannot cause infection.
In addition, the vaccine is an activated vaccine. That means that its purpose is to cause the vaccinated human body to form its own antibodies (the human body is ‘activated’).
What types of HPV vaccines are there and how are they different from one another?
Theoretically speaking, there are 3 different types of HPV vaccines.
The ‘original’ Gardasil – product of MSD – protects against 4 strains of the virus: 6/11/16/18 (two of which are “high risk” strains, and 2 that are “low risk” strains). This vaccine became unavailable when Gardasil 9 was introduced.
Gardasil 9 – product of MSD – protects against 9 strains of the virus including 6/11/16/18/31/33/45/52/58 (seven of which are “high risk” and 2 that are considered “low risk”)
Cervarix – product of GSK – protects against 2 strains 16/18 (“high risk” strains). This is also no longer available since the introduction of Gardasil 9.
So, this means the only vaccine currently available is Gardasil 9.
Which age groups and genders were/are able to receive these vaccines?
Gardasil 4:
Girls and women ages 9-45 years
Boys and men ages 9-26 years
Gardasil 9:
Originally it was approved for ages 9-26 years
Most countries now offer it for people aged 27-45 as well.
Cervarix:
Girls and women aged 9 and above
Boys and men – not registered
Is one of these vaccines preferred over the other?
Absolutely.
When all three different vaccines were available, there was a clear preference for Gardasil 9. In fact, it reached a point where there was actually no practical need for the other vaccines and that is why they are no longer available. Therefore, from here onwards I will be focusing on data regarding Gardasil 9 in my post.
How experienced is the world with the vaccine Gardasil 9?
The vaccine was approved in 2006 and was gradually incorporated into the medical market around different countries in the world. It has been in use in the United States since June 2006.
The vaccine is part of the routine vaccine schedule in many countries, including Australia, the US, the UK, England, Belgium, Canada, Germany, Brazil, New Zealand, Norway, Sweden, Spain, Switzerland and more…
Up until 2017, about 270 million doses of HPV vaccine had been administered around the different countries in the world.
How effective is Gardasil 9?
Randomized controlled clinical trials that ran over a span of several years demonstrated high efficacy both in prevention of infection, caused by the strains that the vaccine covers, as well as prevention of development of genital warts, and a reduction in the development of precancerous lesions.
The efficacy of Gardasil 9 was assessed on tens of thousands of boys and girls worldwide.
Now that over 10 years have passed since the introduction of the vaccine around the world, there are lots of studies out there that demonstrate its efficacy in the real world (not just in research).
Research has shown that one can reach maximal efficacy if they get vaccinated prior to exposure to the virus (prior to sexual intercourse).
In terms of efficacy, the following have been demonstrated:
– A 90% reduction in the risk of infection by viral strains that are covered by the vaccine (6/11/16/18)
– A 90% reduction in development of genital warts
– An 85% reduction in the development of severe precancerous lesions in the cervix.
Today there is already evidence of lower prevalence of cancer caused by HPV in vaccinated women compared to unvaccinated women. In men, the vaccine has demonstrated a 90% reduction in prevalence of genital warts and about 75% reduction in the prevalence of precancerous lesions in the anus, caused by one of the 4 viral strains against which the vaccine provides protection.
Who is this vaccine recommended for?
The vaccine is recommended for males and females ages 9-26.
Why administer it at such a young age? As I already mentioned, the highest prevalence of infection with HPV has been found to occur immediately after the start of sexual intercourse. Also, the highest efficacy of the vaccine seems to occur when the vaccine is given prior to sexual intercourse.
In the United States the vaccine is routinely given at ages 11-12 years for both girls and boys.
What about people over the age of 27? They can, obviously, also receive the vaccine but it is best to focus on people/communities that are at high risk of continuous viral exposure such as those with multiple sexual partners, those who have a different sexually transmitted disease, those who have been sexually assaulted, men who have sexual intercourse with other men, etc. Refer to your national vaccine guidelines to find out if you are among those advised to receive the vaccine.
What if I know that an adolescent aged 12 will not be having sexual intercourse in the next year or so? Is it worthwhile waiting before administering the vaccine?
This is a very legitimate question that I get asked quite often.
I think that even if the parents are sure that their son/daughter will not be having sexual intercourse in the next year, it is preferable to get them vaccinated at this age.
In the past, when we were still waiting for Gardasil 9 to get approved, it made sense to wait a year until it was approved in order to receive a more efficacious vaccine. But as there is currently no better vaccine out there, there is no point in waiting and I think it is important that all adolescents get vaccinated in time.
Another perk for those getting vaccinated at the age of 12 is the ability to receive only 2 doses, as the immune response is better at this age.
Is it possible to vaccinate a person who has already had sexual intercourse or has already been infected with HPV?
The answer is yes. Not all those who have had sexual intercourse have got infected and not all those infected have been infected with viral strains covered by the vaccine. And so, there is nothing to lose when vaccinating this population.
Vaccinating those under the age of 45, who have already developed genital warts and have had pathological pap smears, is also advised, despite the fact that the vaccine will not be protecting these individuals against the viral strains that they have already been exposed to.
Where in the body is this vaccine administered?
This vaccine is administered intramuscularly, in the arm.
How many doses of vaccine does one need to receive to be considered fully vaccinated?
It depends on the age at which the person is receiving the vaccine.
Adolescents under the age of 15 require 2 doses, at least 5 months apart (if the second dose is administered less than 5 months from the first dose, then a 3rd dose is required).
Adolescents over the age of 15 need to get 3 doses. The minimal time interval required between the first and second dose is 4 weeks and that between the second and third dose is 12 weeks (the minimal time required between the first and third dose is 16 weeks).
There are claims that giving 2 doses provides better immune protection, is it true?
It is true. There are several good scientific articles that have demonstrated effective immunity when one dose (instead of two) or two doses (instead of three) are administered to different age groups.
There are several health organizations around the world that have moved to administering less doses of the vaccine.
What if I have only received one (or two) doses of the vaccine?
The rule of thumb for vaccine series that haven’t been completed is that there is no need to start over. Instead, just continue from where you left off, taking into consideration the minimum timeframe required between doses, as mentioned earlier.
For example, a 17.5-year-old female who wants to be fully vaccinated and received her first and only dose before the age of 15 but hasn’t received any doses since needs to simply receive one more dose as soon as possible to be considered fully vaccinated.
How can a parent know whether their child has received the vaccine?
By taking a look at their vaccine records.
Due to low compliance with this vaccine during school, and because many children have not received the full series, I advise all parents to try and find out whether their child is fully vaccinated.
What about those who are fully vaccinated to Gardasil or Cervarix but haven’t received Gardasil 9? Do they need to get vaccinated again?
If you have already received all doses of one of the previous vaccines, then there is no need to get the new vaccine.
If you are still interested in receiving the extra protection that Gardasil 9 provides, you can certainly get vaccinated.
What about children that only got part of the vaccine schedule for Gardasil or Cervarix? Should they complete the series with Gardasil 9?
When completing a vaccine course that has already been started it is preferable to do so using the newest and best products available. Currently, the best HPV vaccine is Gardasil 9, completion of series with Gardasil 9 is advised, even if the previous doses received were Gardasil or Cervarix.
How long does Gardasil 9 protection last?
The Gardasil vaccine was first marketed in 2006. It has been 16 years since, and so far, the vaccine has demonstrated 16 years of protection.
Long term follow-up studies are being conducted to assess whether a booster dose is required.
What are the vaccine’s possible adverse effects?
The common adverse effects are local side effects (pain, redness and swelling). Local side effects are more common after Gardasil 9 when compared to Gardasil 4.
Headaches, dizziness, general malaise, muscle pain, joint pain and abdominal pain have all been reported, starting the day of vaccine administration and up to 15 days later.
Young women are advised to lay down when receiving the vaccination as there have been reports of fainting following vaccine administration in this population.
If the adolescent is supposed to receive the Tdap vaccine at the same time I would recommend getting each shot in a different arm. Keep in mind that the tetanus vaccine is painful, especially for those who have received a different dose.
What about the autoimmune effects that have been reported?
In 2013, Professor Yehuda Sheinfeld, a rheumatologist from Sheba Medical Center in Israel published a paper about several cases of autoimmune disease outbreaks following HPV vaccine administration. However, temporal association does not infer causation, and the authors of the publication concluded that long-term monitoring of larger groups of vaccinated people is required.
To my delight, research conducted before and after 2013 demonstrated that there is no difference in prevalence of autoimmune diseases in vaccinated vs. unvaccinated populations.
Furthermore, in 2017 the world health organization confirmed the safety of the HPV vaccine. This was a conclusion they had reached after having reviewed all the different studies that had been performed regarding HPV safety as well as the 270 million vaccines that had been administered worldwide at the time.
Who cannot receive this vaccine?
Individuals that have a known allergy to one of the components of the vaccine or those who developed an allergic reaction to a previous dose of the vaccine.
What is my practical recommendation?
My recommendation is Gardasil 9 for those ages for which it has been approved. Routine vaccine administration at the age of 11-12 years as offered in most countries in the world.
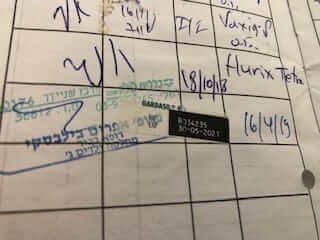
And I practice what I preach. See the picture here to my signature on my eldest daughter’s vaccine record for Gardasil 9.
Is it possible to receive this vaccine together with other routine vaccines? And if so, then how?
Gardasil 9 can be administered together with all the other routine vaccines, including Tdap. If giving them on the same day, administering Tdap and Gardasil 9 each on a different arm is advised.
What if I/my child did not receive the HPV vaccine during the routine vaccine scheduled time?
Refer to your primary care physician or your national health website to find out where and how to receive the vaccine.
Good luck!
For comments and questions, please register
