Herpes infection in children (mainly primary herpetic gingivostomatitis)
The full names of Herpes viruses are Herpes simplex virus type 1 (HSV1) and Herpes simplex virus type 2 (HSV2). There is a wide spectrum of symptoms for these two viruses, ranging from severe neonatal infections, sexually transmitted genital infections, brain inflammation (encephalitis) to rashes and mucosal involvement.
However, the purpose of this article is to summarize the most common presentations of this virus in children which is mucosal membrane and skin involvement. An important medical condition in children which is missed in many of the cases.
The herpes family
There are eight viruses in the herpes family that cause diseases amongst children and adults. However, this section will focus on HSV1 and HSV2. The difference between HSV1 and HSV2 is that HSV1 tends to cause recurrent disease on mucosal surfaces (mouth and/or nose), whereas HSV2 tends to burrow in genitals. Despite this general tendency, both viruses can appear in both regions.
Before we begin, it’s important to discuss terminology surrounding HSV1 and HSV2 infections.
What is primary and non-primary infection?
Primary infection – the first time a child (or adult) encounters this virus. Since the child doesn’t have performed antibodies for this virus, primary infection tend to be more severe.
Non primary (reactivation) – the second or third (or in my case, the hundredth!), time that this virus causes a disease amongst a child (or adult). Reactivation can occur with all of the herpes viruses since these viruses remain dormant (latent) in our bodies after a primary infection. Reactivation may be triggered by certain situations which we will discuss later. However, since the body already has performed antibodies, these infections tend to be much milder or even asymptomatic.
How does the herpes virus spread?
One may contract the virus after being in direct contact with an infected secretion. The problem is this is true even for a completely asymptomatic person who doesn’t even know that they are shedding the virus. I go on to venture that many readers of this very article have herpes in their saliva without any other symptoms! Obviously it is more likely for an outbreak to occur amongst schoolbag children after a case of symptomatic herpes, but it is hard to do source control since infection can occur through asymptomatic individuals as well. It is interesting to note that although a low socioeconomic status is associated with herpes infections, anyone can catch this virus. In fact, research shows that most people were infected by the virus by the age of forty, whether they know it or not.
What’s the common presentation of herpes in children or what is primary herpetic gingivostomatitis?
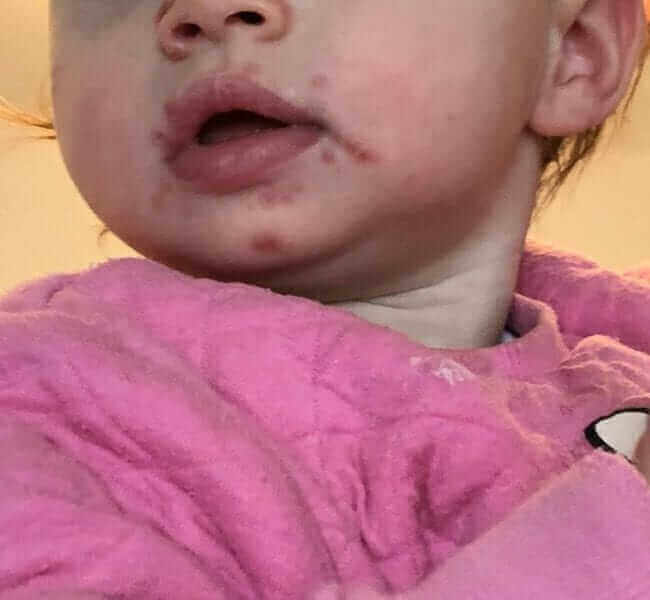
The most common disease is called primary herpetic gingivostomatitis, which is a primary infection that usually appears between the ages of 6 months to 5 years old, and its largely due to HSV1. The child usually has fever and oral cold sores. These children may have difficulty eating and often drool with severe halitosis (bad breath). Sometimes there are cold sores outside of the oral pharynx known as satellite lesions, especially along tracts of saliva. See the first picture.
An experienced pediatrician can easily differentiate herpes from the clinically similar viral presentation of hand, foot and mouth disease caused by Enterovirus (read more here) due to the fact that herpes tend to be a more severe, often causes cervical lymph nodes to be swollen and tender, as well having classic gingival involvement, such as the tendency to bleed after micro-trauma. Herpes often causes a “positive tongue depressor test”, which is when gentle contact during mouth examination with a tongue depressor (a.k.a a popsicle stick), causes a minor bleed. Not to mention, that the classic signs of enterovirus (e.g. rash on limbs) will be absent.
The disease usually lasts for a week. If the child’s lucky the fever and symptoms will pass after 3-4 days; however, sometimes the symptoms can persist for 7-10 days. Remember that sometimes the primary infection can present atypically or even asymptomatically.
Another presentation of this disease, which is less common in young children, is skin involvement. Usually there is one discrete, classic herpetic lesion that can be found anywhere on the body. See the second picture.
These lesions are often found in children who participate in contact sports such as Wrestling or Judo. In fact, that’s where its name, Herpetic gladiatorum comes from. You can read more about the skin manifestations through this link.
What happens after a primary HSV1 or HSV2 infection?
As previously mentioned, following a primary infection, the herpes virus remains dormant in our body and under certain circumstances can reactivate. Reactivation infections tend to have milder symptoms in comparison to a primary infection. See the third picture.
The reactivation often manifests through a cold sore in the same region as the primary infection, especially on mucosal surfaces and is called herpes labialis. These outbreaks may occur sporadically for no known reason; however, they tend to occur during stressful periods (e.g. family events or an important test), concurrently with another unrelated illness or even after heat exposure. Some people never experience reactivation, and there’s no way to know who will be spared from reactivations.

How is herpes infection treated?
First and foremost – supportive treatment which involves antipyretics and lots of fluids. Sometimes the child during primary gingivostomatitis is in so much pain that they refuse to eat or drink. In these cases, it often helps to administer fluids slowly through a syringe. If that doesn’t work, some children will require intravenous fluids to prevent dehydration.
There is no ideal fluid or food for a primary infection. I suggest to let the child have whatever they are willing to eat or drink with an emphasis on fluids. If a child wants ice cream, then so be it. If the child is craving Herring, all the merrier.
Fortunately, we have an effective anti-viral treatment for this unpleasant disease known as Acyclovir (also known in it’s generic form as Zovirax, read more here). The mechanism for this medication was so brilliant that it earned a Nobel prize. During a primary herpes infection, such as herpatic gingiviostomatitis or herpes gladiatorum, systemic treatment can be instituted as early as possible. This medication comes in a syrup form that’s suitable for young patients. During reactivations that manifest with herpetic sores, topical anti-viral treatment should be initiated as early as possible to minimize the lesion. Single oral doses of acyclovir can be considered for older children or adults who feel that they can predict reactivation. In many cases, preemptive treatment prevents the outbreak. Unfortunately, none of these treatments prevent subsequent reactivations.
There are additional anti-viral medications such as Valacyclovir (Valtrex) and Penciclovir. Feel free to discuss the advantages and disadvantages of each medication with your primary physician.
When can my child go back to school after a herpes infection?
A child can resume normal activities after he feels better and is afebrile with dry herpetic lesions.
So, how can we summarize a primary herpes infection in children?
It’s a virus that causes significant morbidity in pediatrics. Unlike most viral infections that have no specific treatment, effective treatment for herpes exists and should be instituted as early as possible for optimal results.
Till next time….

For comments and questions, please register
