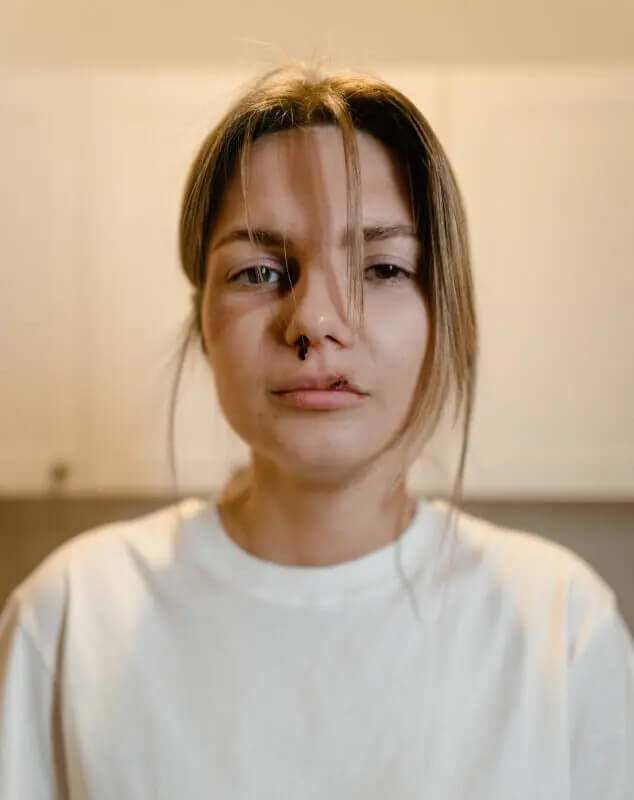
Epistaxis (nosebleeds) in children
A common presentation in children, yet a cause of concern for many parents. But like many other pediatric conditions, there really is no reason for concern when it comes to nosebleeds.
I remember suffering from nosebleeds as a child myself. And see? I turned out alright.
This post has several goals:
1. To provide you with a short explanation about epistaxis – prevalence, types of presentations and causes
2. To overview management of an acute nosebleed in a child and tips on what should be done to handle the situation
3. To share thoughts on the investigation and workup required when a child suffers from recurrent nosebleeds.
So, let’s go ahead and learn what epistaxis means, how to prevent it from occurring and how to manage it if and when it occurs.
What is epistaxis? How common is it?
Epistaxis is simply the medical term used to describe a nosebleed. The origin of the word is Greek. It is an uncommon condition in infants and young children but very common in children aged 3–8 years.
Obviously, it occurs more frequently in the winter months, as a result of the cold and dry weather.
What exactly is the source of the bleeding?
Usually, the source of the bleed is at the front of the nose, closer to the nostrils, in the nasal septum—an area referred to as the “Kiesselbach plexus.” This happens because this area is rich in blood vessels, is located in the front of the nose, and is prone to trauma. It is often scratched or touched by the child, and the mucosa in this region is very thin and easily injured.
In most cases, the bleeding happens suddenly and occurs in one nostril.
When a nosebleed occurs at night, the child may sometimes swallow the blood and later have either bloody vomit or black stools the following morning (due to the blood having been digested in the gastrointestinal tract).
What are the immediate actions one should take if they see a child with a nosebleed?
First of all, keep in mind that most nosebleeds will stop on their own within minutes. Start by pressing on both sides of the nose, on the soft parts under the bone, and tilt the child’s head forward (remember—forward, not backward!).
Try to stay calm, and please do not ask the neighbour to pour a bucket of water on the child.
A cold compress applied to the nose (to restrict blood flow) may be helpful.
If the nosebleed stops within a few minutes, that’s great.
If not, go to the nearest urgent clinic for management with more aggressive therapy.
What if the child just lost a ton of blood?
Even though the nosebleed may seem severe and the child’s bed may appear to be soaked with blood, in the majority of cases, the amount of blood loss is not significant.
Children with a history of coagulation disorders may lose a significant amount of blood as a result of a nosebleed, as you will see below.
What are the causes of epistaxis?
We tend to categorize epistaxis into two types:
Primary epistaxis – this is epistaxis due to an unknown cause and may result from mild coagulation disorders. Other signs that may indicate a coagulation disorder include a family history of nosebleeds or a personal history of prolonged bleeding, such as after injuries, circumcision, or heavy menstruation.
Secondary epistaxis – this type of epistaxis is secondary to trauma, the presence of a foreign object, inflammation, infections (such as viral upper respiratory infections), or chronic use of nasal sprays.
When is investigation advised?
If someone experiences a nosebleed following a blow to the face that stops on its own, then clearly, no investigation is needed.
However, if a child presents with recurrent nosebleeds for an unknown reason, it is important to do the following:
1. Consult with your primary care physician to consider a brief workup, including a complete blood count (more about this here), coagulation function tests, bleeding time test, and von Willebrand factor test. These tests are done via a simple blood draw and require several small tubes.
2. See a pediatric ENT specialist to determine whether nasal cauterization is appropriate.
How can one prevent a nosebleed from occurring?
Try applying jelly-based products or ointments to the front part of the nose. This is especially helpful during the winter months when the nasal passages become dry. If the area appears red and inflamed, some may recommend using an antibiotic ointment to reduce the number of bacteria and help minimize local inflammation.
If a child has a history of allergic rhinitis, make sure it is well controlled. This will help reduce how often the child touches or rubs their nose, which can trigger a bleed.
Additionally, discourage nose picking and try to keep the child’s bedroom humidified, particularly during cold and dry seasons.
Again, for severe or recurrent cases, consult an ENT specialist for assessment and to consider local treatment options.
In summary, this is a very common condition in pediatric medicine. I hope this post provides reassurance to most of you, while also guiding those few cases that may require further evaluation and management by a healthcare professional.
For comments and questions, please register
