The full guide to sinusitis in children (and adults)
One of the more challenging topics to write about is sinusitis. Why? Because it’s a medical condition that doesn’t always follow a clear beginning, middle, and end, and it involves many subjective elements. This is also one of the reasons why so many people confidently self-diagnose with sinusitis—and sometimes, they might even be right.
There are several types of sinusitis, including viral, bacterial, allergic, and mixed forms. It’s not uncommon for patients to say things like, “I know my body—I always end up with sinusitis,” or “When my head hurts this badly, it’s usually sinusitis.” And honestly, it can be hard to argue with them.
To summarize, sinusitis is an inflammation (note: not necessarily an infection) of one or more of the sinuses. The most common causes are bacterial infections and allergies.
Sinus inflammation can lead to significant discomfort and, in some cases, serious complications—both in children and adults.
So let’s explore this topic in detail, and work toward understanding what sinusitis really is—how to recognize it without missing important cases, and how to avoid over-diagnosing or over-treating it.
Let’s Start from the Basics – What Are the Sinuses?
As mentioned in the chapter about rhinosinusitis, the sinuses are air-filled cavities located within the bones of the skull. Their inner walls are lined with a mucous membrane, similar to that found in the respiratory tract. This membrane produces mucus, which drains through small openings into the nasal cavity. When excess mucus accumulates, it can become infected—this is what we commonly refer to as “snot.”
Additionally, the mucous membranes of the sinuses are lined with tiny hairs (cilia) that help move the mucus toward the drainage openings of each sinus.
What Is the Function of the Sinuses? Why Do We Have Them?
That’s a good question. I must humbly admit that the exact function of the sinuses is not fully understood. However, several theories suggest their potential roles in both children and adults:
• Reducing the weight of the skull – especially important in children, as it makes it easier for the spine and body to support the head, which is relatively large in proportion to their body.
• Providing a buffer against head trauma.
• Contributing to voice resonance and tone. If you’ve ever tried to sing with congested sinuses, you’ll understand their impact.
• Playing a role in the growth and shape of the face throughout childhood and adolescence.
What Are the Names of the Different Sinuses and When Do They Develop?
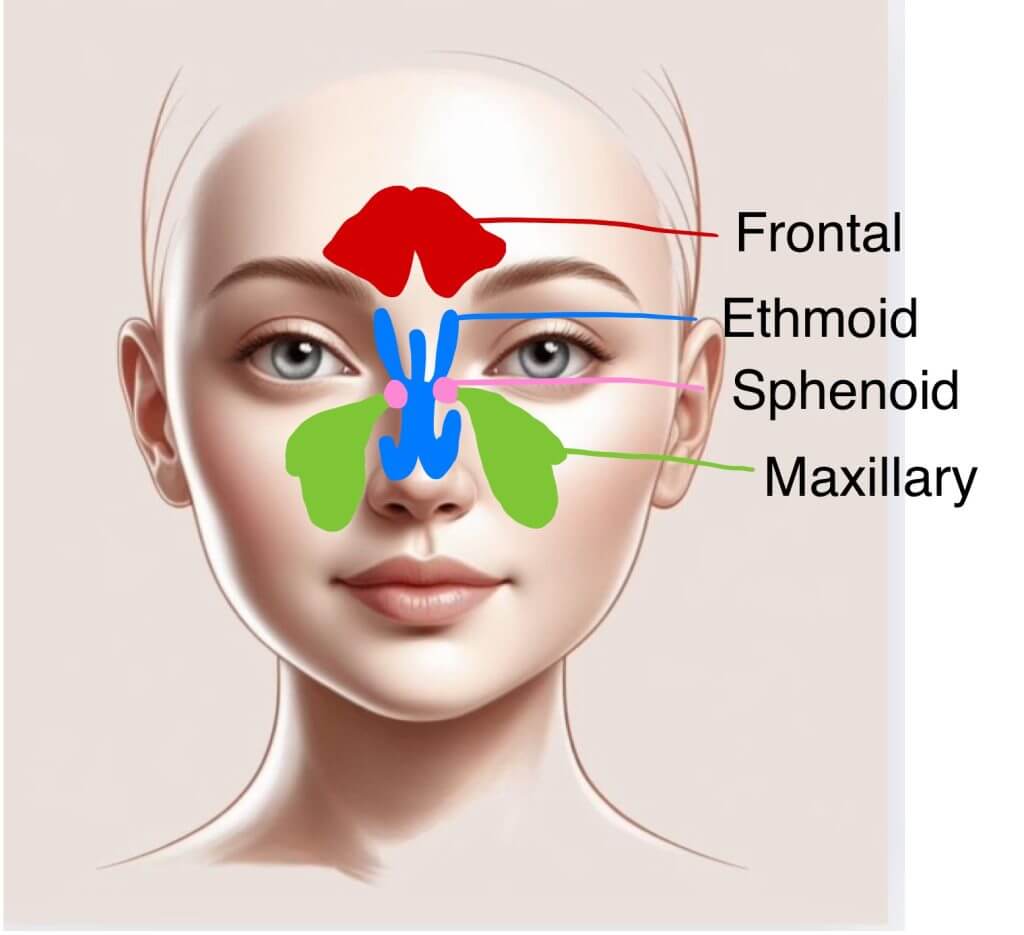
As you read through the descriptions below, refer to the attached illustration for clarity.
The frontal sinuses (in the forehead, above the eyebrows) – these begin developing around ages 7–8 and are fully formed by adolescence.
The maxillary sinuses (on either side of the nose, behind the cheekbones) – these are present at birth but begin functioning and become air-filled around age 4. These are the sinuses most commonly involved in infections.
The ethmoidal sinuses (between the eyes) – these are already air-filled and active at birth.
The sphenoidal sinuses (behind the eyes) – development typically begins around age 5.
What Does “Development of the Sinuses” Mean? Can Children Have Sinusitis?
As you’ve seen, sinuses develop over time in both size and aeration—from early childhood through adolescence. As a result, sinusitis is generally more common in older children and adults.
However, young children and even infants can develop sinusitis in the sinuses that are already air-filled at their age.
Wait a Second, Doc – What Was This Entire Introduction For? What Is Sinusitis?
Simply put, sinusitis is inflammation of the sinuses.
This inflammation may be caused by an infection or by non-infectious factors (most commonly allergies). It can also be classified as either acute or chronic, as we’ll explore further below.
So, If I Have a Runny Nose, Does That Mean I Have Sinusitis?
This is an important question, and understanding the answer is key as we move forward.
The answer is—yes.
In most cases of the common cold, there is some involvement of the sinuses. MRIs conducted on children with runny noses have shown congestion and swelling (edema) of the mucous membranes in the nose—signs of sinusitis—in approximately 68% of cases.
Let’s talk more about children: they typically experience upper respiratory tract infections 6–8 times per year, while adults average about 2–3 times annually. Based on these numbers, the global incidence of sinusitis is enormous.
Fortunately, the majority of these cases are viral and do not require specific treatment. Our role as physicians is to identify the small percentage of cases—estimated at 0.5–2% in children—where the sinusitis is bacterial and requires intervention. So, how can we identify those cases? Let’s explore that next.
Is There a Specific Classification for Sinusitis Based on Duration?
Yes—this classification is quite useful:
Acute sinusitis – This type lasts less than one month and is the most common. It typically develops a few days after a mild upper respiratory viral infection and resolves spontaneously in most cases.
Sub-acute sinusitis – Lasting between 1 to 3 months, this form is often a direct continuation or complication of acute sinusitis.
Chronic sinusitis – This refers to inflammation that persists for longer than 3 months.
While most people experience acute sinusitis, recognizing the different types is important for proper diagnosis and treatment, as each may involve different underlying causes—including distinct bacterial infections.
Let’s Move On – How Does Sinusitis Develop?
In essence, sinusitis results from an obstruction of the sinus drainage pathway. It’s all about drainage. I often tell my patients, half-jokingly, that when it comes to sinusitis, a plumber might be more helpful than a doctor.
Inflammation can cause obstruction—and obstruction can lead to inflammation—making it a classic “chicken and egg” situation.
Here are some common causes of sinus drainage obstruction:
• Infections (viral, bacterial, or fungal) – the most common cause, especially in children.
• Allergic conditions – those with allergic rhinitis or asthma are at higher risk due to nasal congestion.
• Anatomical abnormalities – Some adults experience prolonged and recurrent sinusitis after every mild cold. This could be due to a structural issue in the sinuses that predisposes them to chronic or recurrent episodes. In such cases, imaging studies (like a CT scan) and ENT consultation are recommended.
• Thick mucus – as seen in conditions like cystic fibrosis, which prevents effective drainage.
• Immotile cilia syndrome – a congenital disorder affecting the function of mucosal hairs, impairing mucus clearance.
• Allergic reactions – including allergies to medications, environmental irritants, or fungi.
• Smoking and smoke exposure – a major risk factor.
• Long-term exposure to chemical irritants – which can inflame the respiratory tract.
• Immunodeficiency – weak immune responses increase vulnerability.
• Inflammatory diseases – such as Wegener’s granulomatosis or sarcoidosis.
• Facial trauma or prior surgery – which may interfere with sinus drainage.
• Obstructions – such as nasal polyps or foreign bodies.
• Dental infections – particularly those involving upper teeth, which can extend to the maxillary sinus.
How is Sinusitis Detected?
In short – through a combination of medical history and physical examination.
It is important to distinguish between true sinusitis and a simple upper respiratory tract infection, such as a common cold.
Accurate diagnosis is critical because colds do not require antibiotics—and as you’ve seen throughout this site, we strongly advocate for the responsible use of antibiotics.
How Can You Tell if a Simple Cold Has Progressed into a Bacterial Sinusitis That Requires Treatment?
This is perhaps the most important—and most challenging—question.
At the onset of symptoms, it is often difficult to differentiate between viral and bacterial sinusitis. The duration of symptoms is a key clue.
If symptoms persist beyond 10 days, or if there is initial improvement followed by a secondary worsening within a week, bacterial sinusitis may be suspected.
Patients typically present with worsening congestion and a productive cough.
In some cases, purulent (pus-like) nasal discharge may appear, either unilaterally or bilaterally.
Fever is not always present, and when it is, it is usually mild.
Other symptoms can include halitosis (bad breath), hyposmia (reduced sense of smell), and periorbital swelling.
Diagnosis often relies heavily on the physician’s clinical judgment, as symptoms may be subtle or overlap with those of viral infections.
What About Headaches or Tenderness When Pressing on the Sinuses?
These signs are more common in adolescents and adults than in young children.
They include:
- Headache and facial pain
- Tenderness over the sinuses, often worsened by moving the head or looking down
- Dental pain or gum discomfort while chewing
What About Additional Tests for Diagnosing Sinusitis?
X-rays?
As previously mentioned, MRIs—which are far more sensitive than basic X-rays—often show signs of non-specific, viral sinusitis. Thus, plain facial X-rays are generally considered unreliable and are not recommended.
CT Scans?
CT imaging can provide valuable insights, such as the amount of fluid in the sinuses, mucosal thickening, or drainage blockage. However, CT scans still cannot reliably distinguish between a cold and bacterial sinusitis. They are typically reserved for detecting complications or in cases of chronic or recurrent sinusitis.
Endoscopic Examination (under local anesthesia)?
This method involves inserting a small camera into the nasal passages to evaluate sinus drainage. It allows the physician to identify structural problems, such as polyps, enlarged adenoids, or a deviated nasal septum, that might contribute to recurrent sinusitis.
Sinus Aspiration?
While not a routine procedure, this is occasionally performed in hospital settings. An ENT specialist inserts a needle through the skin, bone, or gums to aspirate fluid from the sinus. The sample is then cultured to identify the specific bacteria responsible for the infection. This process takes around 48 hours and is typically reserved for complicated or unresponsive cases due to its invasive nature.
How Is Acute Sinusitis Treated?
Most cases of acute sinusitis are viral in origin and do not require treatment beyond supportive care.
However, when a bacterial infection is suspected—especially if symptoms are severe or persistent—antibiotic treatment may be warranted.
So, Is the Treatment for Sinusitis Always Antibiotics?
This is critical to understand:
a. Most sinusitis cases are viral and do not require antibiotics.
b. If bacterial infection is suspected, appropriate antibiotic therapy should be initiated.
c. In children, there is limited evidence that decongestants or nasal steroids help recovery—though in adults, they are often included in treatment. Nonetheless, I personally support using nasal sprays to aid sinus drainage in parallel with antibiotics.
Which Antibiotic Is Appropriate for Sinusitis?
Treatment varies, but first-line therapy typically involves a simple penicillin antibiotic, most commonly Amoxicillin.
To those who insist—often mid-aisle at the supermarket—that only Amoxicillin-Clavulanic Acid (Amox-clav) works for them, I’d say two things:
a. Please let me finish my grocery shopping in peace.
b. You may have been misdiagnosed—or the infection could have resolved with a simpler antibiotic. Broad-spectrum antibiotics such as Amox-clav or cefuroxime should be reserved for complicated cases or those involving resistant bacteria.
How Is Chronic Sinusitis Treated?
Chronic sinusitis is less common and should be managed by an experienced ENT specialist.
In these cases, a wider range of bacteria must be considered, and a more tailored diagnostic and treatment approach is necessary.
What About Allergic Sinusitis?
Especially in older children and adults, sinus inflammation can sometimes result from allergies rather than infections.
In such cases, evaluation by a pediatric allergist or ENT may be appropriate to investigate possible allergic causes and guide management.
Is Sinusitis Contagious?
True bacterial sinusitis is not contagious.
However, the viral infections that often precede or trigger sinusitis (such as colds or the flu) are indeed contagious.
When Can a Child Return to School or Daycare After Sinusitis?
A child may return to regular activities once they are feeling well, regardless of whether they are still completing a course of antibiotics.
In Summary, this was no easy chapter to write—but an important one.
I hope it has helped clarify how to recognize and manage sinusitis, and how to make informed decisions together with your physician for the wellbeing of your child.
Good luck!
For comments and questions, please register
