Everything you need to know about bronchiectasis – a chronic respiratory infection in children and adults
Okay so this website has become very comprehensive, so comprehensive that sometimes its content gets quite specific and quite professional.
This topic about bronchiectasis is an example.
Generally, bronchiectasis is a condition involving the respiratory tract, that is characterized by an irreversible widening of the airway and this could be due to many different reasons. This condition can be seen in all the different ages, from childhood to elderlies, and is caused by a variety of different factors, as you will see below.
Up until the past decade, this important condition was not very known, not even among respiratory physicians around the world, and that is why it was slightly deprived of attention.
But in recent years a database with different patients from Europe and America was put together, and there have been many investigative and management research studies that have been carried out.
Let me make this clear. This is a very important condition, and correct management, by a professional in the field, can significantly improve quality of life and life expectancy.
The following topic will be presented to us by Dr Adi Dagan, a senior specialist in pediatric pulmonology and head of the field of bronchiectasis in children and adults.
How common is bronchiectasis?
For different reasons, this condition has become more and more common, and today it can be found in up to 0.5% of the general adult population. That means it is the third most common pulmonary condition, after asthma and COPD.
Nonetheless, even today, it is still underdiagnosed and patients with bronchiectasis are undermanaged and often complain of symptoms for many years prior to their diagnosis and before an individual treatment is offered for their specific condition.
What forms the basis of the process? What happens to the lungs when bronchiectasis develops?
The respiratory tract is structured in a way that is similar to branches of a tree, and the diameters decrease the further you are from the center. The role of the respiratory tract is to lead oxygen into the cells of the body and release carbon dioxide to the external air, all while cleaning the lungs from any environmental dirt that we breathe in everyday, including soot, dust, viruses and bacteria that are in our surroundings. This cleansing occurs with the help of natural secretions and small hairs (called cilia) that are found on the cells of the respiratory tract and expel the dirt out in a symmetric manner. When, for some reason, there is a prolonged inflammation or obstruction of the airways, the wall of the tract and the small hairs are damaged, and this can affect their function and cleansing role.
What are the signs and symptoms of the condition?
The main symptoms are a prolonged, daily productive cough and recurrent respiratory tract infections.
How is this condition diagnosed?
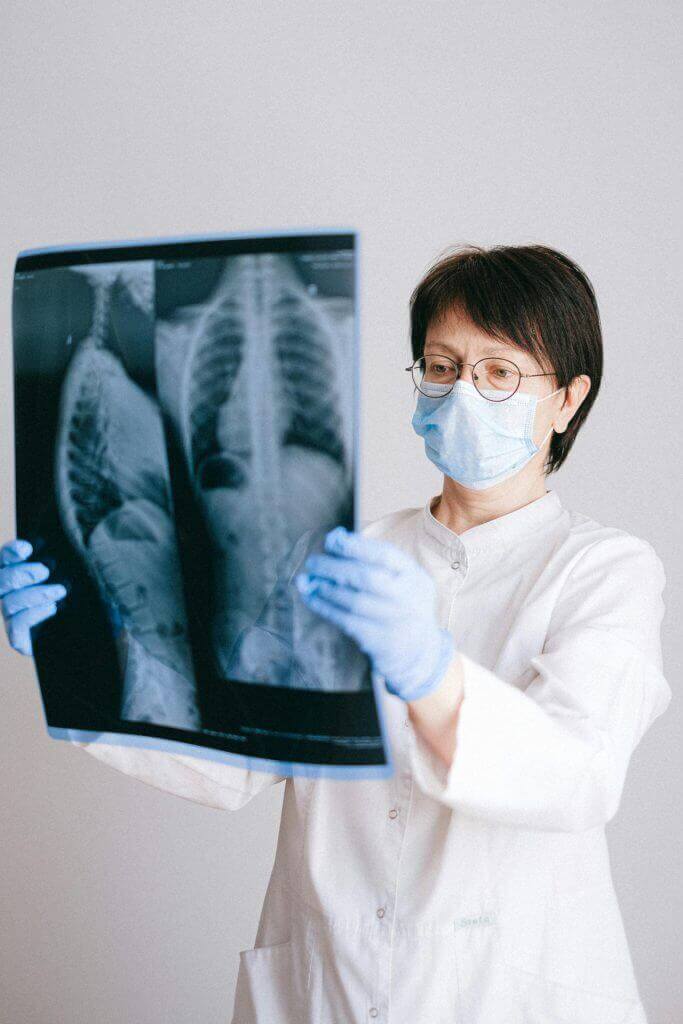
In order to diagnose the disease in a patient with suggestive symptoms, the physician has to request a chest CT, where they will be able to see the expanded respiratory tract and the characteristic secretory plugs.
A chest x-ray is not diagnostic for this condition but can suggest the possibility of this disease when an area with a chronic consolidation is seen, and this means that one should proceed to performing more precise imaging (in the form of CT in this case).
What is the reason for the cause of bronchiectasis?
The causes of this disease are variable and can be divided into two separate groups:
1. Congenital diseases such as primary ciliary dyskinesis or cystic fibrosis, where there is difficulty with expulsion of secretions from the airways and accumulation of chronic inflammation. When these are suspected there are special tests that can be done as well as genetic testing.
2. Primary immune deficiencies (whether they are congenital or acquired) or secondary (such as following chemotherapy for oncological disease or prolonged treatment with steroids that weaken the immune system), and as a result, recurrent lung infections.
3. Medications that cause damage to the airways as a side effect, such as chemical or biological drugs and conditions that occur following bone marrow transplant.
4. Inflammatory rheumatological disorders and inflammatory bowel disorders – such as rheumatoid arthritis or Crohn’s Disease.
5. Bronchiectasis following a severe lung infection (viral or bacterial) or after tuberculosis infection. This is the most common cause of dilated airways. Find out more about lung infections in children here.
What are the main goals of a pulmonologist when diagnosing and managing a patient with bronchiectasis?
Several roles:
1. Identifying the cause of the disease, in order to find the right treatment for the patient’s individual condition
2. Adequate treatment and improvement of daily quality of life of the patient by reducing the respiratory symptoms such as cough and secretions
3. Adequate treatment that will prevent respiratory worsening and medical deterioration which could potentially cause hospitalization and a reduction in pulmonary function to the point of respiratory insufficiency and sometimes the need for lung transplant.
Who should be examined by a pulmonary specialist?
A pulmonologist consult is required for children or adults any age suffering from recurrent respiratory infections or experiencing a productive cough for a prolonged period of time. We are all aware that there are other possible relevant diagnoses, sometimes they are more common (I have already mentioned asthma, read more here), but allow the consultant to think along with you and to give you the right diagnosis.
What happens when bronchiectasis is suspected?
If the physician suspects an irreversible respiratory tract condition – they will refer the patient to a CT test. At this point, after bronchiectasis diagnosis is made, one can refer to a clinic that specializes in the field.
Afterwards, different investigations are carried out depending on the patient’s specific case and history, their physical examination and their risk factors. Most patients will be sent for primary investigations that will include bloodwork, primary screening tests to rule out significant immune deficiencies or cystic fibrosis or undiagnosed rheumatological diseases.
In addition, they will be offered pulmonary function tests to assess the baseline respiratory function and a respiratory physiotherapist’s assessment to teach the patient how to remove their own secretions.
All patients, at all ages, are to test their sputum for bacterial and fungal cultures that can worsen the existing inflammation. If the patients are unable to provide secretions for cultures, usually a bronchoscopy will be carried out so that the airways can be visualized, washed, and specimens sent for cultures.
How is bronchiectasis in children or adults managed?
In terms of treating the existing condition, the treatments available for the population of people diagnosed with bronchiectasis is mainly teaching them how to self-clean their airways on a daily basis and prevent the accumulation of secretions that could cause worsening of the inflammation. This can be done with the help of hypertonic saline nebulisations for softening the secretions and physiotherapy exercises, with or without special devices, individualized to the patient.
The other treatments available are more individual – depending on the patient’s clinical status and the reasons for their disease and also depending on the bacteria or fungi that grow in their phlegm. Many of the systemic disease have their own specific therapies and their goal is to reduce inflammation. When there are respiratory exacerbations, there is a need for antibiotics in order to prevent deterioration and hospitalizations due to respiratory infections. There are patients who have frequent exacerbations that take prophylactic anti-inflammatory medications for prolonged periods of time.
Nowadays, there are more and more research studies about new biologic medications that are intended to reduce the frequency of infections and chronic inflammation in the airways by acting against the inflammatory cells and the cytokines (that initiate inflammation) that are secreted in mucous.
In summary, this is a very significant disease, no matter what age it presents at. Fortunately, in recent years there has been tremendous development in the field of bronchiectasis and our ability to detect it and manage it has greatly improvement. We even have a world bronchiectasis day, created to increase awareness.
If you suspect you may have this disease, see a specialist for a consult.
Good luck.
For comments and questions, please register
