Neonatal jaundice
One of the issues that occupies parents the most in their newborn’s first few days of life is jaundice.
Many people are familiar with the fact that this is a common phenomenon, and that it usually resolves without the need for any treatment and does not cause any harm.
Nonetheless, jaundice needs to be monitored because in certain severe and rare cases, it can cause harm.
Also, seeing an improvement in your baby’s jaundice is an indication of health and wellness, as you will learn below.
The aim of this post is to discuss and explain jaundice and to answer any questions that you may have with regards to the need for monitoring and treatment. Be aware, however, that this post may seem simple and straightforward on the one hand, but complex on the other. You will find a lot of important terminology here.
So, wash your face and turn your phones on silent. You’re about to turn into those parents that know absolutely everything in medicine, including everything about jaundice.
How common is jaundice in newborn babies?
The answer is: very common.
About two-thirds of newborns will have jaundice after birth. In premature babies, it is even more common and can be seen in up to 80% of infants. So, some level of jaundice will be seen in most children out there.
What causes jaundice? What is bilirubin?
The yellow colour that you may see in a child’s conjunctiva (the white part of the eye), is a result of an accumulation of a substance called bilirubin that contains a yellow pigment. This substance is formed in the human body by a natural process during which red blood cells are disassembled. The bilirubin formed makes its way to the liver and undergoes a series of processes in the liver cells, its chemical nature changes and it is later excreted through the bile ducts into the intestines.
So, how does bilirubin accumulate? This can occur either as a result of excessive production of bilirubin, a problem in one of the processes in the body that deal with bilirubin or an issue with its dissemblance and excretion out of the body.
Is jaundice dangerous?
The change in the skin’s colour, on its own, is not dangerous. But the change in colour is a sign of accumulation in the body, including the brain.
A large accumulation of bilirubin for a long period of time can cause neurological damage (a disease called Kernicterus), and that is the reason why jaundice in neonates is worthy of attention and monitoring.
In fact, the reasoning behind all repeat bilirubin measurements conducted on infants is the search for that 1% that are at high risk of reaching very high levels of bilirubin in the blood, which may be dangerous, and to treat them adequately immediately, as you will learn below, to prevent the potential harm that bilirubin can cause.
How do you check for bilirubin in neonates?
Let’s starts with the units – these are always in milligrams per decilitre. As these units are universal, from here on I will not mention the units when I mention bilirubin values. Now let’s get back to our question: how can we measure the level of bilirubin in the blood?
Clinically – by observing the baby and checking to see whether he has a yellow colour.
Jaundice spreads from the head downwards. Generally speaking, one can see yellow pigmentation of the face and conjunctive when values are above 5 in the blood. The more yellow the infant is in the lower parts of their body, the higher the level of bilirubin in the blood (yellow skin below abdomen indicates a level of approximately 15). Sounds easy right?
This has been studied extensively, and it was shown that even the most experienced of physicians, nurses and mothers are not always able to correctly predict the bilirubin levels. And in dark skinned children – it is even more difficult.
Transcutaneous measurement – Since the clinical estimation is not accurate enough, we have several devices that may be of help. The transcutaneous device is inserted on the infant’s forehead or chest and with the help of different techniques (depending on the intensity of the colour), it is able to read the bilirubin levels in the blood. This device will yield results that are very similar to the real value of bilirubin in the blood. It is excellent for screening and monitoring since it gives a good sense of how severe the jaundice is but it is not 100% accurate and its accuracy has a tendency to decrease the higher the bilirubin value is (15 and above), the darker the skin colour and also in infants who have undergone phototherapy (see below). Even though these devices may yield incorrect measurements, their use can still be very helpful in giving the medical team an estimation of the severity of the jaundice without having to draw blood, and by doing so, enable the team to make decisions about the next step of action.
Blood tests – the level of bilirubin in the blood can be measured one of two ways:
The first technique is a heel prick. The blood squeezed from the heel is placed in a glass tube called a capillary tube.
The second technique is a regular venous-prick. Venous blood is then collected into a regular blood test-tube.
Generally speaking, we tend to believe that the venous bilirubin levels are 1-2 units higher than the ones collected in the blood from the heel. However, in practice, we use the heel technique much more often, especially if bilirubin levels need to be checked every day.
Heel-pricks and capillary tubes, however, are not always available as opposed to the venous-blood option. In addition, when taking venous blood, we also have the option of measuring additional parameters that may be needed for workup.
The measured bilirubin levels are then compared to the Bhutani curve (I will explain more about this below) and the level of severity and required follow-up is determined.
Are there different types of neonatal jaundice?
There are, and it is very important to understand the different types. There are also several different ways to divide the types of jaundice.
The main division, the more important and practical one, is direct and indirect jaundice.
What do these two means?
Remember how we said that bilirubin (the substance that accumulates in jaundice) undergoes several chemical processes in the liver? Well, the main process is the transformation of this substance into one that can dissolve in water and be excreted from through the biliary tract into the intestines, and from there, outside of the body through stool.
The accumulation of bilirubin up until that process, where it becomes dissolvable in water, is called direct jaundice. The accumulation of bilirubin past that stage, is referred to as indirect jaundice.
The terminologies ‘direct’ and ‘indirect’ originate from the lab techniques that are used to check for the different types of bilirubin.
These different types of jaundice have different causes.
The “regular,” and more common neonatal jaundice, is the indirect type.
I will teach you more about direct jaundice later on in this chapter but this is the time to say that direct jaundice is never physiological and indicates and underlying illness that needs further workup.
Another important classification to be familiar with is ‘physiological jaundice’ (=originating from normal processes occurring at an increased rate, cannot cause harm) and pathological jaundice (=originating from a processing that could be related to disease or an abnormal state and could potentially cause harm). The difference between jaundice that is referred to as physiological and one that is pathological is the onset of presentation, the rate at which the bilirubin rises and its severity. See more below.
What is physiological jaundice?
Let’s start with emphasizing, once again, that physiological jaundice is always a result of indirect bilirubin.
The level of bilirubin in our body naturally rises after birth, and so jaundice will present in the first 2-3 days of life. The level of bilirubin peaks around the 4th-5th days of life and then disappear. The reason for the jaundice is an accumulation of the substances formed when fetal red blood cells are broken down and the lack of maturity of the chemical processes that occur in the liver that turn bilirubin into a substance that can be excreted through the biliary tract.
So, when on the one hand there is an excess production and on the other hand a lag in its clearance – the bilirubin accumulates in the blood and jaundice appears. The rise can be slower and may last for longer. In physiological jaundice, the bilirubin levels are low and so there is no need for any treatment or monitoring. When this natural process is “messed up” or is “too much” we get pathological jaundice and the bilirubin accumulates. I’ll get into this in more detail below.
How do we know that the bilirubin levels are relatively low? We use a curve called Bhutani (named after the doctor who created it) and it shows us the normal bilirubin levels relative to age. As I have already mentioned, if you take a look at the curve you will see that as the baby gets older, he is “allowed” to be more yellow. The graph peaks at around 6 days of age, and after that we expect the bilirubin levels to start decreasing in physiological jaundice.
It is also important to see that the graph is divided into levels of risk. What are these exactly? The higher the baby’s bilirubin levels the greater the risk that the jaundice will worsen and reach levels that require treatment and follow-up.
What is pathological neonatal jaundice?
pathological jaundice the rate at which the bilirubin levels rise is greater than the normal increase (as seen in physiological jaundice). This includes:
– Jaundice that presents in the first day of life.
– Jaundice in which the rate of bilirubin increase is high (more than 5 units/day).
– Jaundice that reaches high risk levels.
– Jaundice that lasts longer than 10-14 days after birth.
– And direct jaundice – this is less common (physiological jaundice is always indirect whereas indirect jaundice is always pathological).
All these types of jaundice have a list of causes and possible reasons. A good pediatrician will be able to navigate the workup in the correct and intelligent direction.
Are there risk factors for development of high bilirubin levels/pathological jaundice?
Yes. Some babies may have risk factors that lead them to high bilirubin levels. The following babies will need to have their bilirubin levels measured more frequently:
– Babies who develop jaundice on their first day of life.
– Babies who develop jaundice that reaches high risk levels (as seen on the curve).
– Babies born prematurely.
– Babies whose blood types are different to their mother’s blood time – this is true only to mothers with blood type O. Mothers with blood type O carry antibodies against all the other blood types. That is why people with blood type O are able to donate blood to everyone but can only receive blood from those with blood type O. These antibodies can cross the placenta, cause destruction of red blood cells in the baby and become the cause of accumulation of excessive bilirubin. Despite the fact this blood type incompatibility is seen in 15% of pregnancies, the process I just mentioned will occur only in about 0.6% of these pregnancies. Let me just say that there are other causes of red blood cell destruction by antibodies, but I’m not going to get into that (for example the difference between positive and negative blood types, etc.)
– A sibling that received phototherapy for jaundice.
– A huge hematoma – this is a source of red blood cell destruction that leads to a rise in bilirubin.
– Exclusively breastfeeding – especially if the breastfeeding isn’t going well and the baby is not feeding properly and gaining weight – see more below.
– Certain ethnicities – especially children whose parents are of Asian origin and this is because of genetic differences in enzymes responsible for the processes occurring in the liver.
– G6PD deficiency/fava bean allergy – how is this related? If you read about fava bean allergy in the following link here, you will learn that this condition can lead to red blood cell destruction and can be the reason behind high bilirubin levels in the blood. In some countries, newborns are tested for this during their first couple of days of life, before they are discharged from the hospital.
– High protein levels in the infant’s blood – bilirubin is carried in the blood by a protein called albumin, and low levels of this protein cause the bilirubin to be released into the bloodstream.
– Infants that undergo asphyxia during birth – a condition where there is a lack of oxygen delivery to the blood.
What is jaundice that is related to breastfeeding?
I suppose everyone knows that infants who are breastfed tend to have jaundice. But why is this? There are two main reasons/two main types:
– Breastfeeding jaundice – this is the early-stage jaundice, and it is an ‘exaggeration’ of the process that I described that occurs in physiologic jaundice. This type of jaundice presents in the first week of life in infants that are breastfed. On average, infants that are breastfed have higher bilirubin levels that infants that are bottle-fed (formula). Breastfeeding jaundice occurs due to insufficient breastmilk intake that leads to insufficient weight gain as well as the milk itself (will explain more about this below).
– Breastmilk jaundice – this is the late-stage jaundice; jaundice that presents in a small percentage of breastfed infants after their first week of life and it leads to higher levels of bilirubin that last for longer, sometimes even several weeks. The reasoning behind this jaundice is confined to the characteristics of the breast milk which contains an enzyme that turns bilirubin in the intestines back into its indirect form and by doing so increases its absorption back into the blood.
So, should you not breastfeed? Should you stop breastfeeding because of the jaundice?
No, no and no!
Breastmilk is the best “formula” out there for most infants. Even in those with breastfeeding jaundice and breastmilk jaundice. Of course, the primary care physician should be consulted, and the infant should be weighed. In most cases, there will be no need to add formula to the baby’s diet just to bring down the bilirubin levels if it is not at a dangerous level. Doing this will probably only mess up the child’s breastfeeding routine and habits. See more below about the rare times when the mother might be advised to do this.
I’m going to just try and make this a little clearer because I do not want infants whose mother read these posts to see their doctor at the age of 3 weeks, with completely yellow babies and not having gained a gram of weight. It is important, especially in breastfeeding infants, to see the primary care physician in the first few days of life and have their baby weighed.
And do not worry, I will be getting to the issue of circumcision soon.
What does the workup for jaundice consist of?
The words “jaundice workup” are often heard at the hospital.
It is as simple as it sounds. The workup for jaundice is carried out when pathologic jaundice is suspected. It just means that your baby will undergo a series of tests so we can try and figure out the possible cause of the jaundice.
What does it include?
– A complete blood count that assesses whether the level of red blood cells in the blood is within or below normal limits. Because as I mentioned earlier, in jaundice there is an increased destruction of red blood cells.
– A test that checks whether the jaundice is direct or indirect. As I mentioned earlier, each one of these may have different causes.
– A test for blood type and crossmatch with maternal blood, which checks for any maternal antibodies that may have crossed the placenta and caused destruction of red blood cells in the baby. Remember how we learn about the maternal blood type and how it is related to jaundice?
– G6PD enzyme levels – a deficiency in G6PD causes increased destruction of red blood cells and a quick rise in bilirubin levels. See? You’ve got this!
– And sometimes a few other tests, depending on physician discretion, to try and rule out other differentials to the cause behind jaundice.
How is neonatal jaundice treated?
It is important to remember that the goal behind treatment is to identify those babies that are at higher risk of developing severe jaundice to prevent the rare cases of bilirubin accumulation at high levels that may cause neurological damage to the baby.
The truth is that the most important part of management is follow-up. By following up on the infants, you can be sure that no one “escapes” the office with high bilirubin levels, and if they do so then it is not for too long. That is the reason why prior to discharge from the nursery in most countries, all infants undergo jaundice screening test using the transcutaneous device. This is also the reason why parents are advised to see their pediatrician within two days after discharge. Please make sure you do so.
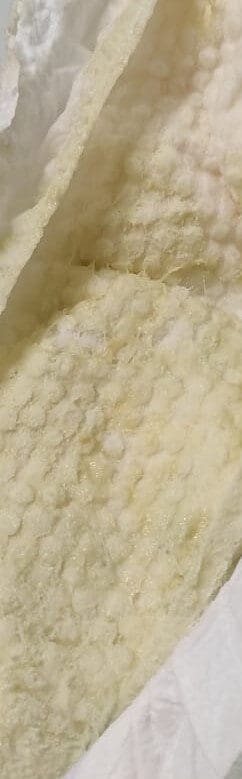
The pediatrician will ask lots of questions about the history of the pregnancy, the delivery, the birth weight, the maternal blood type (many mothers get tested for their blood type), the infant’s feeding habits, the infant’s stool colour (see the important image below) and the frequency of all the risk factors that we discussed earlier. Afterwards, he will examine the infant, assess the severity of jaundice, weigh the infant, and measure the bilirubin using the transcutaneous device, if needed. If the value on the device is high, the pediatrician will refer you to a heel-prick blood test or a venous blood test, depending on what is available at the time (the heel-prick method isn’t available everywhere). Depending on the results, the pediatrician will determine whether there is a need for further workup and the frequency of monitoring required to ensure that the bilirubin does not reach levels that require treatment.
For bilirubin values that do not require any special management other than monitoring, there are a number of things that you can try to decrease the chances of reaching high values:
– Make sure your child is feeding well – this is really the most important management. If your child is breastfeeding, make sure the breastmilk is sufficient and that he is gaining weight. If need be, see a lactation consultant to help improve your technique. If your child is bottle-fed, make sure he is receiving sufficient amounts of formula in adequate frequency. Read more about how much does a baby need to eat here. When needed, especially if your child is not gaining enough weight, consult with your nurse or pediatrician. Infants who are not feeding properly and gaining enough weight will have prolonged jaundice that is more. Take a look at this post here to read more about important issues with regards to the beginning of a baby’s life.
– Observe your baby’s stools – remember how we said that bilirubin undergoes changes when it is in the liver and gets excreted into the intestines? In the intestines, some of the bilirubin can turn back into the original bilirubin and get absorbed into the intestines and the blood. In babies who pass stools infrequently, their stool sits in their intestines for longer and this allows more bilirubin to be absorbed back into the bloodstream. An infant who is feeding well will usually pass stool more frequently and thus his/her bilirubin levels will decrease.
What should not be part of the treatment of jaundice?
Of-course, this question is also important.
– Do not expose an infant to the sun as an alternative to phototherapy – this is unhealthy and can be dangerous.
– Do not stop breastfeeding altogether – the jaundice that most breastfed infants will get will not lead to anything dangerous. Beyond missing out on all things that are good in breastmilk, the difficulties that cutting off breastfeeding could lead to in terms of feeding habits, slow weight gain and even dehydration, the severity of jaundice will only deteriorate. Therefore, encouraging breastfeeding and improvement of the technique, together with a follow-up of weight gain is all that needs to be done. The only time breastfeeding should be stopped is if the bilirubin reaches very high levels that continue to increase and reach values that require plasma exchange (see more about this below). Even then, the cessation of breastfeeding should be temporary, and the mother can continue pumping breastmilk in the meantime.
– Do not give the infant sugar water instead of food – why? There is absolutely no need for this. An infant needs food and calories and not sugar water and it only prevents them from eating and gaining weight and it worsens the jaundice.
Treatment of jaundice at the hospital
In addition to all the simple treatments suggested above, there are several other treatments that can be provided to the infant.
Phototherapy
I’m sure you’ve all seen babies with jaundice “tanning” under a purple light, with sunglasses (to protect their eyes) in the nursery. So, it’s not exactly a tanning bed. This therapy is referred to as phototherapy. It is a simple and common form of treatment for jaundice when it reaches a certain level, depending on the age of the infant. The therapy is based on the discovery that a certain wavelength of light can cause a chemical change in bilirubin that allows it to be excreted into the intestines and urine and by doing so decreases the level of bilirubin in the blood. Nice and simple.
How do you know when a baby needs phototherapy? So, similarly to the Bhutani curve that I mentioned earlier, we have other charts that guide us as to when an infant’s bilirubin levels require phototherapy, depending on their age. Phototherapy is administered for several hours during which the bilirubin levels in the blood of the baby are measured several times, until they are below the threshold required for treatment. After the baby has reached such a value, phototherapy is stopped but the bilirubin levels continue to be monitored because there is a concern for rebound.
Generally speaking, phototherapy does not have any big side effects. However, during the therapy the baby may develop a self-resolving rash, a change in temperature or slight dehydration (in an infant that isn’t feeding well) that can be treated with fluids etc. Phototherapy does not have any known long -term effects or complications.
Intravenous Immunoglobulins – antibody therapy
When the reason behind the jaundice is maternal antibodies that have crossed the placenta and have caused destruction of the baby’s red blood cells, and when the jaundice continues to increase despite maximal phototherapy, the baby is given a large intravenous load of antibodies that “block” the maternal antibodies and prevent the destruction of the baby’s red blood cells.
Plasma exchange
The last line of treatment for jaundice.
When the bilirubin levels continue to rise despite intensive phototherapy and they reach values that are very high, plasma exchange is carried out. Just like the name states, a certain volume of blood is exchanged with matched blood for the blood bank and by doing so bilirubin is simply removed from the blood. The procedure has possible complications, and we try to avoid it as much as possible with the help of the treatment options I mentioned before. Not done very often.
Should circumcision be delayed because of jaundice?
Medically speaking, if your pediatrician believes that your child’s jaundice is physiological and is not related to a liver disease, a significant destruction of red blood cells or any other significant medical problem that requires workup and treatment then there is no reason for you not to proceed with circumcision because of the infant’s jaundice (there may be reasons other than jaundice for why circumcision should be postponed, see more in this link here).
Furthermore, if the jaundice is indeed not dangerous, then the actual bilirubin value that was measured is not significant either. I know that many Rabbis want the baby’s bilirubin levels to be below 12 or 12.5 or even 15 (they each have their own cut-off) but this has no medical basis and medically speaking it does not matter whether the baby’s bilirubin is 10.7, 11.8, 12.9 or 13.4 when the jaundice is uncomplicated and not dangerous.
It is true that at higher values of bilirubin, pathological jaundice that requires meticulous monitoring and treatment should be considered, as I mentioned earlier.
What should we do with an infant who has jaundice and has been discharged from the hospital?
Now that we have learned all the material related to jaundice, let’s try and summarize what needs to be done practically.
Remember how before discharge the babies undergo screening tests for jaundice with the help of the transcutaneous device?
– If the device yields a high value, a blood test is done and the parents are told when they need to do a repeat test, depending on the results (according to the Bhutani curve):
o Low risk – clinical follow up within 48-72 hours at the pediatrician’s office who will then decide whether a repeat test is required (either transcutaneous or blood test).
o Low intermediate – clinical follow up within 48 hours at the pediatrician’s office, who will then decide if there is a need for a repeat test (transcutaneous or blood test).
o High intermediate – this risk level requires a repeat test within 24 hours and a workup for jaundice as we mentioned above.
o High risk – this requires an immediate laboratory workup as well as determining whether phototherapy and continuous monitoring of bilirubin levels several hours later at the hospital are needed.
– Some babies are treated with phototherapy during hospitalization. These babies also usually undergo a workup for jaundice and the parents receive a set of guidelines from the hospital regarding the next bilirubin test depending on the results of the workup that was done.
– If the values are not high, you will be told when you should see your pediatrician. The usual recommendation is within two days. At the pediatrician’s office the child will undergo his first checkup and the pediatrician will determine the need for either a transcutaneous test or blood test, depending on the intensity of jaundice and the chances of developing severe jaundice. After receiving the first results, the pediatrician will determine the need for follow up measurements according to the classification I mentioned above.
– An infant who has significant jaundice in their second week of life will need to undergo blood tests to measure the level of bilirubin and a complete blood count. At bilirubin levels below 13, there is no need for repeat tests. If the bilirubin values are between 13 and 15, the infant will be asked to return for follow up within 48-72 hours. Values above 15 require a full laboratory workup as I mentioned above.
– Prolonged jaundice – jaundice that lasts for longer than 2 weeks needs to be assessed. One should make sure that a jaundice workup, similar to the one I mentioned, was carried out and sometimes additional tests are also required to rule out the various causes of jaundice. And this is certainly also true for jaundice that lasts 3 weeks or 1 month.
One more word about direct jaundice
I’ll just say this one more time – direct jaundice is always pathological and always requires a workup. If the baby has direct jaundice, he needs to undergo a workup to rule out infectious disease, diseases that are related to the bile ducts and diseases related to the proper metabolism of substances in the body. Practically speaking, this means a physician’s assessment and a quick and effective follow-up.
You parents do not need to guess whether your child has direct or indirect jaundice. This is something that can be tested for, if need be.
But you parents still have an important job, so listen up.
A very important clue into problems within the biliary tract is the appearance of white stools (acholic stools). I’ll remind you that the colour of the stool comes from fluids that are excreted through the biliary tract and into the intestines, and mix with the stool. An infant who has a problem with their biliary tract is unable to excrete bile properly and so their stool is white, see the image below. So, if your child is passing white stools, without any yellow or green pigment, take a photo of their stool and see a doctor immediately.
In summary:
this is a long chapter that covers a super common issue in babies. In most cases, jaundice is self-resolving but because it could also indicate a different problem in the baby, it requires monitoring.
For comments and questions, please register
