Reflux (spit-ups) in babies
There’s a legendary post on this site, which defines very clearly four common reasons for restlessness in babies, (link here):
- Colic (there is also a specific post on this subject on the site, right here)
- The “hungry” baby.
- A baby with cow milk protein allergy (there is also a specific post on this subject on the site, right here).
- A baby with gastroesophageal reflux disease (occult reflux), see also here.
I hope you are not reading this post because your baby is restless. Let me start by reminding you about that post, just so we can speak in the same language (since definitions are very important).
Reflux – spit-ups. The baby is cute and vital, and has lots of spit-ups. Not something to get excited about.
Reflux disease – when the spit-ups, or just acid from the stomach going up through the esophagus, creates a problem.
So you must read carefully and understand these definitions so you won’t get confused, go on wrong directions and give your child the wrong treatment.
What is reflux and why is it common in babies?
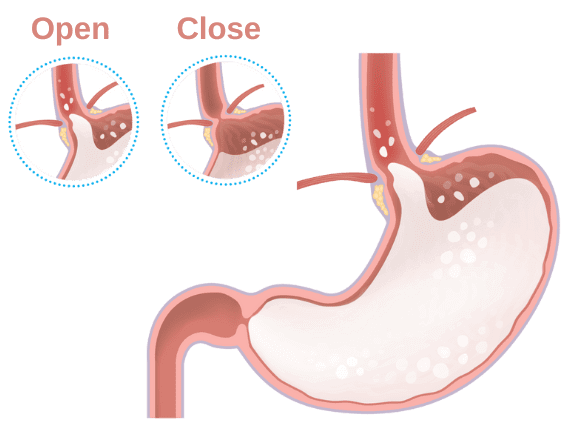
Reflux or gastroesophageal reflux (GER), is essentially a regurgitation. Stomach content is going up through the esophagus to the mouth. Since at this stage of life the muscle between the esophagus and the stomach is not quite developed, stomach content can easily rise from the stomach to the esophagus (see in the enclosed figure). Reflux is physiological and happens every day in all babies. Sometimes it will be accompanied with spit-up and sometimes not.
Again, this is a normal condition that happens in all babies. A baby with simple reflux is not in pain, and is not restless, so we call him – “the happy spitter”.
How common is reflux (GER) in babies, and when will it be over?
Sub-clinical reflux, without spit-ups happens in all babies.
Reflux with spit-ups happens in a lot of babies.
According to the textbooks, reflux is common in the first few months of life, reaches a peak around 4 months and is over by 1 year of age.
In real life – GER is more common up to 4 months, and after that the prevalence drops. Most children who suffer from reflux (with or without spit-ups), are cute, healthy and have no pathology (and therefore are called “happy spitters”).
What is gastroesophageal reflux disease (GERD)?
Reflux disease or gastroesophageal reflux disease (GERD) is when the reflux creates a medical pathology, such as:
1 – Failure to gain weight – not common, but sometimes you see babies who spit-up large quantities of food and fail to thrive and gain weight.
2 – Heartburn (occult reflux) – with or without spit-ups, the acidity in the stomach goes up to the esophagus and the baby is in pain and suffers, mainly during meal times. These are the babies I talk about in that other post about restlessness in babies.
3 – Respiratory symptoms – due to passage of stomach content to the lungs. Not common.
How do you diagnose reflux (spit-ups) in babies?
Does your baby have spit-ups? Then he has reflux or GER.
Is he healthy? With no significant restlessness episodes? Does he thrive and gain weight? Then he is a “happy spitter”.
Other diagnostic examinations include X-rays with or without contrast, Ph-metry, impedance or endoscopy and are unnecessary in most cases.
What is the treatment in cases of babies with reflux?
First you need to understand that this is a very common physiological condition, harmless and not dangerous. Second, there is room for changing some habits, especially those related to eating:
1 – There is no need for frequent feeding of the baby. I wrote about “over feeding” in another post on the site. I see about 50 babies who eat less than what they need, before I see one who eats too much. Over feeding is a very pathologic and very uncommon condition. On the other hand, there is no need to give a 180 ml bottle every hour just because the baby made a little noise.
2 – Do not feed the baby in a bassinet or in a sitting position. These are positions that can worsen reflux.
3 – After you feed a baby with reflux it’s important to hold the baby in an upright position, without placing your shoulder against his stomach.
Burping – is not a must. If he did burp– great! If he didn’t burp after 15 minutes, you can move on.
4 – If the baby is awake and under your supervision you can put him in a prone position, when the head of the bed is elevated at a 30 degree angle. Remember that the bed needs to be elevated using objects outside the bed (like placing two heavy books under the legs of the bed). You can elevated the head of the bed during the night, when the baby is asleep, but remember that babies needs to sleep on their back, to lower the risk for Sudden infant death syndrome (read more here).
5 – Prevent exposure to smoking – you’d be surprised, but exposure to smoke will increase the risk for reflux in babies.
If you did these behavioral changes and the baby keeps spitting, then you can consider thickening agents or changing the formula.
When and how to change formula, for a baby with reflux?
This is a complicated answer.
First of all, if the baby is breast fed, then the recommendation is to continue breast feeding. Remember that thickening of food (AKA pumping milk and then adding thickening starch for example) is very complicated and mostly not recommended. You can try to breast feed in an upright position, while leaning back.
If the baby eats formula, you have two options –
1) Changing formula to anti-regurgitation (AR) formula. AR formula are formulas based on cow milk protein, and a thickening agent such as starch – based on potatoes, rice or carob powder. When the formula reaches the acid content of the stomach, the starch will turn into a thick mass and regurgitation of the food is less likely.
2) Thickening the existing formula. Remember that thickening the food means increasing the amount of calories in the amount of food the baby consumes. It would make the baby gain weight faster. Most of the time this is unnecessary.
Remember that sometimes, when changing formula to AR formula or when thickening the existing formula, there can be some changes in the baby’s bowel movements – constipation or just discomfort (as in other cases of changing formula). In most cases it will get better with time. To avoid these situations, try changing the formula gradually in the course of a few days.
Are there any medications that can help with reflux?
The answer is no.
If someone says to himself – “Omepradex”, then he must read this post from the beginning. Omepradex helps with heartburn (occult reflux), and not with “simple” reflux. Other medications, which were used liberally in the past (such as antacid or similar products), are out of the question.
Any other recommendation for babies with reflux?
As I wrote in another post on the site, I think every baby and every family who are experiencing difficulties regarding food and eating habits, needs to consider along with their pediatrician, starting with solid food at an early age. You can read about this more in this post.
So in conclusion, what did we learn?
A lot. On what is reflux (called also GER). What is the difference between reflux and gastroesophageal reflux disease (called also GERD). On the treatment options for reflux. On thickening formula, including AR formulas.
Good luck!
For comments and questions, please register
