Pneumonia in children
Wow, what a difficult chapter to write.
This is a massive topic and I have so much information that I want to pass on to you. I need to really think to myself what it is that I want to emphasize here.
Here goes my first message. During winter it seems like every other kid that complains of fever and cough to his doctor, leaves the office after having been diagnosed with pneumonia. At my department at the hospital, I see kids under the age of one who have already managed to have had “pneumonia” twice or even three times in their life.
Do so many kids really experience that many episodes of pneumonia? Not at all.
So, what are among the main take-home messages that I have for you?
After having read the chapter, I hope you are able to answer the following questions:
1. What is the real definition of pneumonia? And what infections do not fall under that definition?
2. What are the two types of pneumonias in children (and adults)? What is the difference between them? What is the appropriate treatment for each?
3. How can you reduce the chance of your kid getting this unpleasant illness?
Can adults also learn something new from this chapter? For the most part, yes. The definitions of pneumonia are similar in both children and adults. However, some of the specifics may vary.
Let’s start. I’m going to need all of your attention.
What will this chapter discuss?
This chapter will focus on discussing pneumonia in children of all ages, who have no significant past medical history and are usually healthy.
This chapter will not discuss pneumonia in children with immunosuppression (neither acquired or congenital) nor will it discuss pneumonia in children with significant congenital pulmonary or cardiac malformations or children with chronic diseases. It is true that some of the definitions throughout this chapter may also apply to such children, but the general approach to children with chronic diseases is different.
In addition, this chapter will discuss community-acquired pneumonia, and not the type of pneumonia acquired through hospitals.
What is pneumonia?
This is an infection of the lung parenchyma.
It is a significant illness, mainly in children under the age of 5 years. It is the illness that causes most deaths worldwide, but mostly in developing countries. Nonetheless, it is clear to all of us that these days, with the availability of vaccinations, antibiotics and the utmost medical care, there is no reason for mortality from community-acquired pneumonia in developed countries.
Listen to this anecdote – at the rare times when I diagnose a child with pneumonia at my clinic, I see the fear in the adult’s eyes (usually grandparents, not young parents). Why? Because some of them still remember how difficult and fatal pneumonias used to be many years ago.
Is pneumonia an illness caused by bacteria or viruses? What is the difference between the two?
A real pneumonia is one that is caused by bacteria.
Typical pneumonia – caused by certain types of bacteria
Atypical pneumonia – caused by other bacteria.
All the other diagnoses given by physicians, including viral pneumonia, bronchitis, bronchiolitis, “the virus has found its way down to the lungs”, and all sorts of other strange things, all describe viral infections that do not meet the definition of pneumonia. Even if upon auscultation the physician is able to hear a concert of sounds across the lungs, including wheezing, crepitations and whatnot – there could still certainly be pulmonary involvement, but the infection is a viral one of the lower respiratory tract (lower respiratory tract infection), and not a real infection, like the ones we are learning about in this chapter. If you’d like to read a summary of the all the different winter-illness diagnoses in children, including what it means to have an URTI, an LRTI, bronchiolitis etc., I suggest you read this post here.
So, let’s just get this straight – viruses do not cause real pneumonias.
What types of bacteria cause pneumonia?
Now that we are all on the same page, we can divide pneumonias into two. There are different bacteria responsible for the different pneumonias.
Typical pneumonia – the most common bacteria causing this pneumonia is Streptococcus pneumonia. Others include Group A Streptococcus, Staphylococcus aureus, and Hemophilus influenza type B.
Atypical pneumonia – the most common bacteria causing this include Mycoplasma pneumonia and Chlamydia pneumonia.
Which one is more common, typical or atypical pneumonia?
I’ll tell you more about the differences between them below but for now I’d like you to just note that typical pneumonia is more common in children under the age of 4 while atypical pneumonia is more common in older children and adults.
What is the difference between typical and atypical pneumonia?
Now that we have understood that different bacteria cause different types of pneumonia, and that viruses can cause pulmonary infections but not real pneumonias, we can recognize that the different pneumonias present differently.
Typical pneumonia – usually occurs in infants and children under the age of 4 years. The presentation is that of high fever and a very ill-appearing child. The child is usually breathing heavily and may grunt and seem hungry for air. Sometimes the child will also have abdominal pain (especially if the pulmonary infection involves the lower lobes of the lungs). In some cases, the child could have a preceding viral illness and the pneumonia could be a secondary bacterial infection, where the bacteria sort of ‘takes over’ the viral infection, causing the fever to spike up further.
This is why we tend to see more pneumonias in winter; there are a lot more viral infections in winter.
This is also why vaccines for viral infections are able to reduce the prevalence of pneumonias.
Usually, there will be a unilateral finding on the side of the lungs where the infection has occurred, upon physical examination by a physician. Remember that even the best of physicians is sometimes unable to find pneumonias upon auscultation and therefore, sometimes, further workup is required even if the lungs sound clear. More about this below.
Atypical pneumonia – usually occurs in children aged 5 and above. This pneumonia is generally a lot more common than the typical pneumonia. The presentation is that of a prolonged cough, sometimes with a fever that isn’t too high.
Findings on auscultation may be unilateral or bilateral (on both sides! Note that this is different compared to typical pneumonia).
So, let’s try to summarize all these differences in a table.
| Typical Pneumonia | Atypical pneumonia | |
| Age | Usually under age 4 | Over age of 5 or adult |
| Presence of fever | Usually yes, high | Not always |
| Preceding illness | Preceding viral infections | Without a preceding viral infection |
| Cough | Yes, purulent | Yes |
| Ill-appearing Child | Most of the time yes | Usually no |
| Findings on auscultation | Unilateral abnormality | Either unilateral or bilateral abnormality |
| Findings on blood work | Elevated blood count and inflammatory markers | Inflammatory markers are not necessarily elevated |
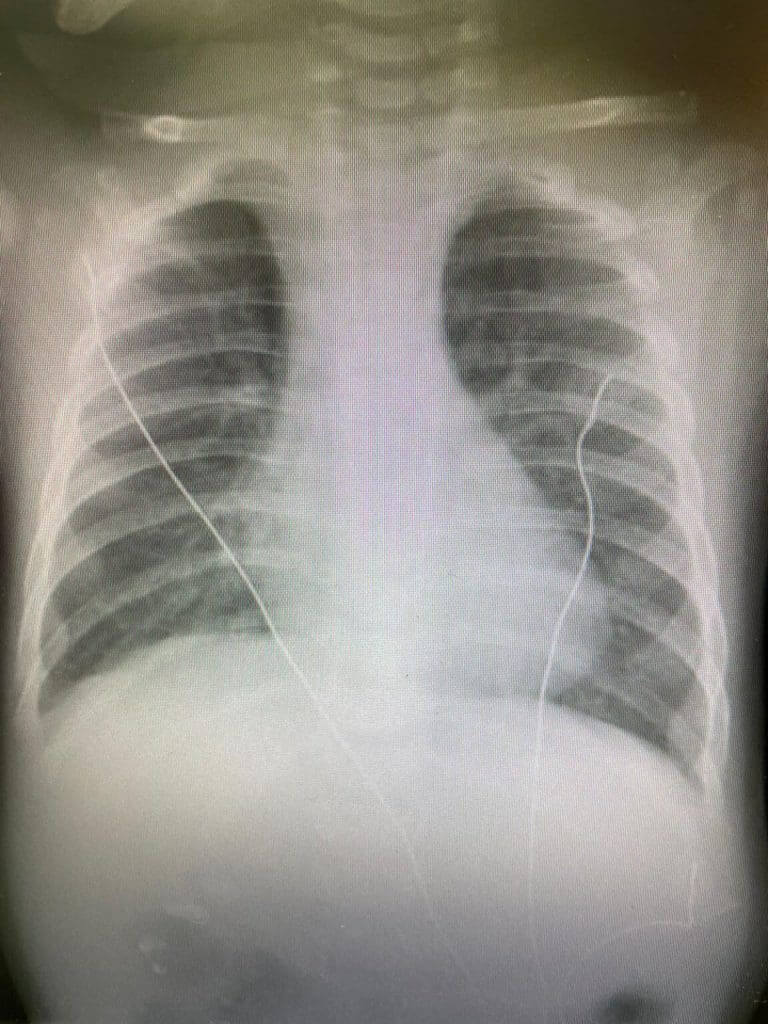
| X-ray | Focal infections | Focal or bilateral infection |
| Antibiotic Treatment | Read more below | Read more below |
So, how is typical pneumonia diagnosed?
Let’s talk about this. What signs in your child should raise concern for pneumonia to you as a parent? How will your doctor know to make the diagnosis?
This is not a simple task, not at all. During winter every other child has a fever of 40 degrees Celsius and a non-stop cough for several days.
Let’s start with the history of the illness – most children with typical pneumonia will be infants and younger children with very high fever and a cough. Sometimes the cough presents only later in the course of the illness, after the child has been put on medication.
The chances of a child without fever having real pneumonia is very, very low.
Ill-appearance and grunting are both signs that should raise concern for pneumonia and they require a visit to the doctor’s office.
Findings on physical examination – generally speaking, physicians know what they are supposed to hear when auscultating the lungs, for them to be able to diagnose pneumonia. Where does the problem lie? Physicians can’t always hear everything well, both due to insufficient cooperation of the children, the noise from their crying and also because some pneumonias are in areas that are more difficult to hear on auscultation.
What findings are inconsistent with a diagnosis of typical pneumonia? Bilateral findings, wheezing, crepitations and desaturations.
So, all those kids that are diagnosed with pneumonia when they have wheezing and low oxygen saturations levels, in reality have viral bronchiolitis, and not pneumonia.
Blood work – in typical pneumonia the complete blood count and the inflammatory markers are elevated (mainly CRP). Read more about CBC here.
Chest X-ray – generally speaking, in a real pneumonia there is a focus of infection, a clear, inarguable, consolidation in one of the lobes. There are no perihilar infiltrates, no bilateral signs, and it is not simply a suspicion. There is a real consolidation on x-ray.
So practically speaking, what should be done to diagnose pneumonia in children?
So again, I’ll only be speaking about typical pneumonia here. A combination of different things are needed for diagnosis. Past medical history, a proper physical examination and in some cases, bloodwork and a chest X-ray.
It is completely legitimate for a pediatrician to suspect pneumonia and not proceed to any further workup once he has listened to the medical history and auscultation is consistent with the diagnosis.
On the other hand, it makes sense for the pediatrician to order a complete blood count for a child with four days of high-grade fever but no findings on physical examination.
If the blood count is high, it would make sense to proceed with a chest X-ray.
This is how many cases of pneumonia are found during the winter months; we call these occult pneumonia.
How can pneumonia be treated in children?
In addition to antipyretics and analgesics, the treatment for pneumonia can be one of two:
Typical pneumonia –the penicillin family of drugs is used with the drug of choice being Amoxicillin. The dose administered has to be high – 80 milligrams per kilogram of body weight (maximum of 1500 milligrams per day), divided into two doses.
The length of treatment depends on the severity of the illness and ranges from 5 to 10 days. Read more about the length of treatment here, in an article that demonstrated that 5 days of antibiotic treatment is sufficient for pneumonia.
Atypical pneumonia – macrolide family of drugs is needed. In children, Azithromycin is used. Read more about azithromycin here.
Of course, in cases where there are complications are suspected, including pleural effusion (pus in the lungs), admission to a hospital and intravenous antibiotic administration will need to be considered.
What about nebulizers and inhalers?
In real pneumonia, there is no need for treatment with nebulizers and inhalers. Viruses are what justify treatment with nebulizers and inhalers.
Therefore, if your pediatrician prescribed your child, who is under 4 years old, with azithromycin for pneumonia as well as nebulizers – this is the time to start asking questions.
How can pneumonia be prevented?
It is obviously not possible to prevent all the different pneumonias in children. Sometimes, it hits you like lightening. But, there is still an important answer to this question and that is vaccines.
Vaccines against bacteria that can cause pneumonia – the pentavalent vaccine includes a vaccine against Hemophilus influenza type B and Prevnar, a vaccine against pneumococcal infections.
Vaccines against viral pathogens that may lead to secondary bacterial pneumonia – influenza, in particular. Read more about the influenza vaccine here.
If there are any adults that are reading this right now – I suggest you also read about vaccines against pneumonia in adults here.
What should a child with recurrent pneumonia do?
First, read this chapter thoroughly.
And then move on to read this next chapter, that will be posted very soon.
So, what have we learned so far about pneumonia in children?
is not so easy to diagnose pneumonia in children.
Both parents and physicians need to know the difference between the different types of pneumonia and mainly to be able to distinguish between viral infections that do not require antibiotic treatment and real pneumonias that require adequate antibiotic treatment.
Good luck!
For comments and questions, please register
