
The baby’s umbilicus
The umbilicus is a relatively “small” topic with a clear start, middle and end.
On the other hand, there’s at least one condition that I’ve seen missed if not treated on time (granuloma), and I would really like to draw parents’ attention to this topic.
What is the umbilicus (belly button) and what is its role?
The umbilicus is that area in the abdomen where the umbilical cord in pregnancy was attached to the fetus from the placenta.
There are three blood vessels in the umbilical cord (two arteries and one vein), and it supplies oxygenated blood from the mother to the fetus and unoxygenated blood back from the fetus to the mother.
The incidence of single artery in the cord is 0.5-1% of deliveries, more so in twins, and although this finding may be a risk factor for diseases in the fetus or for pregnancy complications, in most cases this is an isolated finding and is meaningless.
Of-course, when this finding is identified in pre-natal screens in pregnancy, it warrants referral to a gynecologic consultant, a comprehensive screening in good hands and referral to genetic testing.
The average length of the umbilical cord at birth is 55 cm, and after delivery the midwife places a plastic clip on the umbilicus a few centimeters away from the neonate’s body and cuts the cord above the clip.
Most babies leave the hospital looking similar to picture number 1 with what is called an umbilical cord stump.
Sometimes the clip is removed at a few days of age and then the umbilicus will look a little different (dried).
When does the umbilical stump fall off?
On average at age two weeks, although it’s possible a few good days before or after.
A considerable delay in the falling off of the stump (over a month after birth) is correlated with over-disinfection of the area, see below. In addition, rarely, the delay in its falling off is correlated with infections and problems of the immune system.

Why should the umbilicus be treated in a special way in a baby?
Since the umbilicus and the area around it are open, and this is fetal tissue, it is an easy spot for bacteria to proliferate and cause infection.
How to treat the umbilicus of a baby?
The area should be disinfected with 70% alcohol/chlorhexidine for as long as the stump has not fallen off yet, and a few days following that. Disinfect when changing the diaper several times a day (up to 3 times, no more). Note – excess disinfection may cause a delay in disconnection of the stump and thus, some autoroties claim that no active disinfection should be done. and the umbilicus should be left dry. I still prefer 70% alcohol/chlorhexidine disinfection 3 times daily.
How do you disinfect the umbilicus?
Techniques of cleaning are diverse, I’ll suggest two techniques that may complement one another:
For the gentle – dip a Q-tip (unused…) in 70% alcohol/chlorhexidine and pat the wet tip on the area of the umbilicus.
Less gentle – direct splashing of the alcohol in moderate amount to the area of the umbilicus and cleaning and absorbing with a pad afterwards.
It’s possible to combine the techniques as needed.
Note that the stump may and should be touched gently and moved, patting the Q-tip (or splashing the alcohol) in the entire area of the umbilicus. This action is not painful for the child.
It is common to see discharge in this area, on the Q-tip or otherwise, including bloody discharge. Don’t worry. This is just like an injury at any other place in the body that may bleed a little.
It is possible and necessary to bathe the baby regardless of the status of the umbilical stump. After the bath, the neonate’s skin should be gently dried off, also in the naval area. The upper and frontal part of the diaper touching the area of the umbilicus may cause movement of the stump and mild injury to the area. Try to put the diaper on in a way that minimizes this friction.

What is important to notice in the umbilical region?
Infection – as mentioned above the umbilical region and the stump provide a convenient medium for bacterial proliferation that may cause a local infection (omphalitis) or even more invasive infection (cellulitis and more). How will we recognize the infection? Existence of local redness, swelling and sensitivity, yellow, thick and malodorous discharge (it’s important to smell it, a bad smelling umbilicus equals an infected umbilicus equals a visit to the doctor). See an example of an infected umbilicus in the picture.
An infection may occur also in cases when the umbilicus was treated adequately, and when infection is suspected it should be assessed by a doctor.
The doctor will check and decide whether it should be treated, including local antibiotic treatment (an antibiotic should be chosen to cover the wide range of bacteria that can be involved in this region) or sometimes systemic treatment (oral or IV).
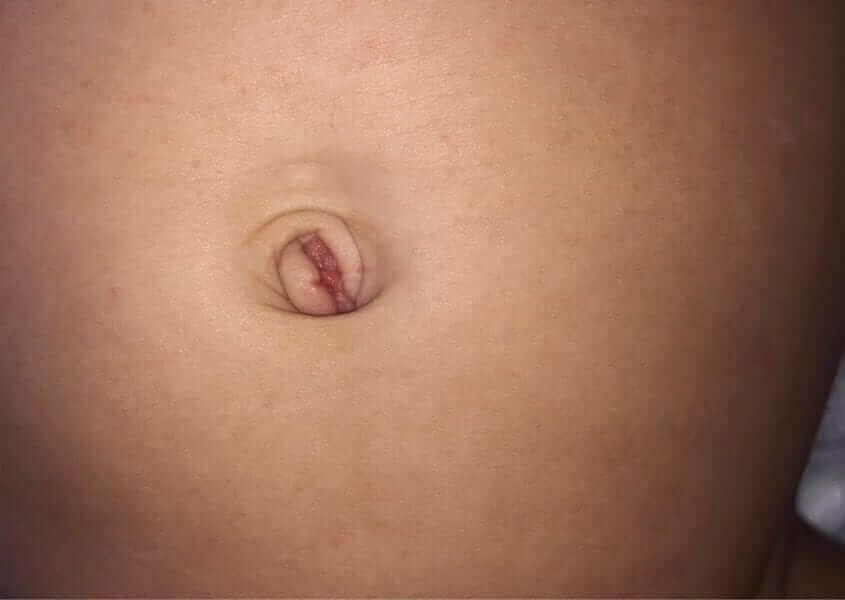
Granuloma – a protrusion in the center of the umbilicus that appears after the umbilical stump has fallen off.
Relatively common and represents an inflammatory response in this area (see picture 4).
The granuloma can be wet/secreting and its main problem is aesthetic (mainly long term).
Therefore, many parent are referred to chemically burn the granuloma. However, early and correct diagnosis may cause it to disappear and prevent the need for intervention.
If the parents identify such a bump, a pediatrician check-up is in order. The treatment at the first stage simple, and be a meticulous disinfection of the area with alcohol.
In addition, it’s possible to consider combining an appropriate antibiotic (there are bacteria of all types in this area including gram positive, gram negative and anaerobic) and a mild steroidal cream.
I recommend alternating between the creams every three hours and within one or two days improvement and diminishing of the granuloma is observed.
What is an umbilical hernia?
Weakness and lack of complete closure of the muscular ring around the umbilicus. The finding is of a soft bulge appearing mainly during a cry or a cough.
It is common in children and the size varies between less than one centimeter and more than five centimeters.
Most of these hernias that appear before the age of 6 months disappear by the age of one year. Larger hernias may also close spontaneously by the age of 5 years.
Large hernias, or those that have not closed after a few years, or are symptomatic, should be examined by a pediatric surgeon to consider surgery to close the hernia.
In conclusion, a small organ that usually doesn’t cause any problems, but early and appropriate treatment prevents trouble even in these cases.
For comments and questions, please register
